
J-Kerner serial key or number
J-Kerner serial key or number
Clinical Focus
- Gastroenterology/Nutrition/Hepatology, Pediatric
- Pediatric Gastroenterology
Professional Education
- Fellowship: Stanford University School of Medicine Registrar (1979) CA
- Residency: Stanford University School of Medicine Registrar (1976) CA
- Medical Education: University of California at San Francisco School of Medicine (1973) CA
- Board Certification: American Board of Pediatrics, Pediatric Gastroenterology (1990)
- Board Certification: American Board of Pediatrics, Pediatrics (1979)
- Internship: Stanford University School of Medicine (1974) CA
Current Research and Scholarly Interests
I am interested in pediatric nutritional support and have experience evaluating new enteral and parenteral products especially for the neonate (I studied a "new" I.V. fat product for Abbott; I participated in a multicenter trial of a formula with fish oil in it for neonates with Mead Johnson and a multicenter trial of a new human milk fortifier for Wyeth). I am the medical director of our nutrition support team and home pharmacy and am interested in short- and long-term "outcome studies" re: use of TPN-impact on development of patient and family functioning in short bowel patients on long-term parenteral/enteral support.
More recently my research has involved : studying how to limit amounts of Aluminum in TPN solutions;Use of ethanol locks in preventing CLABSIs;Use of novel fat emulsions in IR patients; developing a "Care Card"for home TPN patients to improve the healthcare of pts. with central lines who present to the ED with fever;treatment of central line occlusion (original studies of Alteplase); risk factors of CLABSIs in pediatric short bowel syndrome:
Liver biopsies in the first year of life in IR patients on TPN
2020-21 Courses
- Independent Studies (5)
- Directed Reading in Pediatrics
PEDS 299 (Aut, Win, Spr, Sum) - Early Clinical Experience
PEDS 280 (Aut, Win, Spr, Sum) - Graduate Research
PEDS 399 (Aut, Win, Spr, Sum) - Medical Scholars Research
PEDS 370 (Aut, Win, Spr, Sum) - Undergraduate Directed Reading/Research
PEDS 199 (Aut, Win, Spr, Sum)
- Directed Reading in Pediatrics
All Publications
- Getting the OK to Import Zero K MVI: Maintaining TTR in an Infant with SBS.Digestive diseases and sciencesHuang, A., Lee, K., Chan, M., Mak, K., Nishioka, F., Gilbaugh, A., Laguit, K., Nespor, C., Almond, C., Kerner, J.2020
- Risk Factors of Ambulatory Central Line-Associated Bloodstream Infection in Pediatric Short Bowel Syndrome.JPEN. Journal of parenteral and enteral nutritionSeddik, T. B., Tian, L., Nespor, C., Kerner, J., Maldonado, Y., Gans, H.2019
Abstract
BACKGROUND: Children with short bowel syndrome (SBS) receiving home parenteral nutrition (HPN) are predisposed to ambulatory central line-associated bloodstream infection (A-CLABSI). Data describing risk factors of this infection in children are limited.METHODS: Retrospective cohort, single-center, case-crossover study of children ≤18 years old with SBS receiving HPN from January 2012 to December 2016. Univariate and multivariate mixed effect Poisson regression identified the relative risk (RR) of A-CLABSI with proposed risk factors.RESULTS: Thirty-five children were identified; median follow-up was 30 months. A-CLABSI rate was 4.2 per 1000 central line (CL) days. Univariate analysis identified younger age (RR: 0.92 per 12-month increase [95% confidence interval {CI}: 0.85-0.99; P = 0.036]), shorter small intestine length (RR: 0.96 per 10-cm increase [95% CI: 0.92-0.99; P = 0.008]), lower citrulline level (RR: 0.86 per 5-nmol/mL increase [95% CI: 0.75-0.99; P = 0.036]), and recent CL break (RR: 1.55 [95% CI: 1.06-2.28; P = 0.024]) as risk factors for A-CLABSI. Multivariate analysis showed increased A-CLABSI with clinical diagnosis of small intestine bacterial overgrowth (SIBO) (RR: 1.87 [95% CI: 1.1-3.17; P = 0.021]) and CL breaks (RR: 1.49 [95% CI: 1-2.22; P = 0.024]).CONCLUSIONS: Factors influencing gut integrity increase A-CLABSI rate, supporting translocation as an important mechanism and target for prevention. Clinical diagnosis of SIBO increases A-CLABSI rate, but whether dysbiosis or diarrhea is responsible is an area for future research. CL maintenance is crucial, and prevention of breaks would likely decrease A-CLABSI rate.
View details for DOI 10.1002/jpen.1667
View details for PubMedID 31179578
- Delayed appearance of mature ganglia in an infant with an atypical presentation of total colonic and small bowel aganglionosis: a case report.BMC pediatricsSalimi Jazi, F., Chandler, J. M., Thorson, C. M., Sinclair, T. J., Hazard, F. K., Kerner, J. A., Dutta, S., Dunn, J. C., Chao, S. D.2019; 19 (1): 93
Abstract
BACKGROUND: Total colonic and small bowel aganglionosis (TCSA) occurs in less than 1% of all Hirschsprung's disease patients. Currently, the mainstay of treatment is surgery. However, in patients with TCSA, functional outcomes are often poor. A characteristic transition zone in TCSA can be difficult to identify which may complicate surgery and may often require multiple operations.CASE PRESENTATION: We present the case of a male infant who was diagnosed with biopsy-proven total colonic aganglionosis with extensive small bowel involvement as a neonate. The patient was diverted at one month of age based on leveling biopsies at 10cm from the Ligament of Treitz. At 7months of age, during stoma revision for a prolapsed stoma, intra-operative peristalsis was observed in nearly the entire length of the previously aganglionic bowel, and subsequent biopsies demonstrated the appearance of mature ganglion cells in a previously aganglionic segment.CONCLUSIONS: TCSA remains a major challenge for pediatric surgeons. Our case introduces new controversy to our understanding of aganglionosis. Our observations warrant further research into the possibility of post-natal ganglion maturation and encourage surgeons to consider a more conservative surgical approach.
View details for PubMedID 30953480
- Procalcitonin as a Predictive Marker for Bacteremia in Children With a Central Line and Fever.Hospital pediatricsDamman, J., Arias, P., Kerner, J., Zhang, K. Y., Dehghan, M., Krishnan, G., Nespor, C., Bensen, R., Park, K. T.2019
Abstract
Unnecessary use of antibiotics is an increasing problem. In this study, we sought to determine the diagnostic accuracy of procalcitonin in predicting bacteremia in children with a central line and fever, and we sought to determine optimal cutoff values to maximize sensitivity and specificity. This is the largest study to date in which procalcitonin is examined as a predictive marker of bacteremia in pediatric patients with a central line and fever.We conducted a retrospective cohort study of children aged 0 to 23 years with a central line and fever of 38°C who had procalcitonin and blood cultures drawn before initiation of antibiotics and had no other identified bacterial infection. Patients were also prospectively monitored via a custom-built electronic medical record dashboard for eligibility.There were 523 patients and >2500 procalcitonin values reviewed for eligibility. Of these, 169 (47%) patients and 335 blood cultures with procalcitonin were included. There were 94 (28%) positive bacterial blood cultures and 241 (72%) negative bacterial blood cultures. In bacteremic cultures, the mean procalcitonin level was 9.96 ± 15.96 ng/mL, and the median procalcitonin level was 4.85 ng/mL (interquartile range 18.5). In nonbacteremic cultures, the mean procalcitonin level was 1.23 ± 10.37 ng/mL, and the median procalcitonin level was 0.3 ng/mL (interquartile range 0.7). A receiver operating characteristic analysis indicated a procalcitonin level of ≥0.6 ng/mL as the best cutoff point that produced a sensitivity of 85.6% and a specificity of 65.7% (area under the curve 0.85).Procalcitonin is a sensitive biomarker in predicting bacteremia in children with a central line and fever.
View details for PubMedID 31097470
- The Runs: Sudden Copious Ostomy Output in an Acolonic Hirschsprung Disease Patient with Short Gut SyndromeDIGESTIVE DISEASES AND SCIENCESNakayuenyongsuk, W., Barnes, D., Martin, B., Christofferson, M., Kerner, J.2019; 64 (1): 56–59
- Nutritional Needs and Support for Children with Chronic Liver Disease.NutrientsYang, C. H., Perumpail, B. J., Yoo, E. R., Ahmed, A., Kerner, J. A.2017; 9 (10)
Abstract
Malnutrition has become a dangerously common problem in children with chronic liver disease, negatively impacting neurocognitive development and growth. Furthermore, many children with chronic liver disease will eventually require liver transplantation. Thus, this association between malnourishment and chronic liver disease in children becomes increasingly alarming as malnutrition is a predictor of poorer outcomes in liver transplantation and is often associated with increased morbidity and mortality. Malnutrition requires aggressive and appropriate management to correct nutritional deficiencies. A comprehensive review of the literature has found that infants with chronic liver disease (CLD) are particularly susceptible to malnutrition given their low reserves. Children with CLD would benefit from early intervention by a multi-disciplinary team, to try to achieve nutritional rehabilitation as well as to optimize outcomes for liver transplant. This review explains the multifactorial nature of malnutrition in children with chronic liver disease, defines the nutritional needs of these children, and discusses ways to optimize their nutritional.
View details for PubMedID 29035331
- Feeling the Impact of Long-Term Total Parenteral Nutrition.Digestive diseases and sciencesSellers, Z. M., Thorson, C., Co, S., Schaberg, K. B., Kerner, J. A.2017
- Management of short bowel syndrome in postoperative very low birth weight infantsSEMINARS IN FETAL & NEONATAL MEDICINEMayer, O., Kerner, J. A.2017; 22 (1): 49–56
Abstract
Short bowel syndrome is a potentially devastating morbidity for the very low birth weight infant and family with a high risk for mortality. Prevention of injury to the intestine is the ideal, but, if and when the problem arises, it is important to have a systematic approach to manage nutrition, use pharmaceutical strategies and tools to maximize the outcome potential. Safely maximizing parenteral nutrition support by providing adequate macronutrients and micronutrients while minimizing its hepatotoxic effects is the initial postoperative strategy. As the infant stabilizes and starts to recover from that initial injury and/or surgery, a slow and closely monitored enteral nutrition approach should be initiated. Enteral feeds can be complemented with medications and supplements emerging as valuable clinical tools. Engaging a multidisciplinary team of neonatologists, gastroenterologists, pharmacists, skilled clinical nutrition support staff including registered dietitians and nutrition support nurses will facilitate optimizing each and every infant's long term result. Promoting intestinal rehabilitation and adaptation through evidence-based practice where it is found, and ongoing pursuit of research in this rare and devastating disease, is paramount in achieving optimal outcomes.
View details for PubMedID 27576105
- Severe Lactic Acidosis in a Parenteral Nutrition-Dependent Teenager with Ulcerative Colitis.Digestive diseases and sciencesBarnes, D., Kerner, J.2016; 61 (10): 2804-2806
- Iodine Supplementation for Pediatric Patients Receiving Long-Term Parenteral Nutrition.Nutrition in clinical practice Santoro, J. D., Nespor, C., Poole, R. L., Kerner, J. A.2016; 31 (2): 245-249
Abstract
Patients dependent on parenteral nutrition (PN) are among a group at risk of developing iodine deficiency. Supplementation with iodine in this population has been debated in a number of studies, resulting in variable clinical practices. The Committee on Clinical Practice Issues of the American Society for Clinical Nutrition recommends a dose of 1 mcg/kg/d of parenteral iodine for patients receiving PN. At our institution, PN trace elements do not include iodine, although this is not the case internationally. Our study sought to assess iodine levels and thyroid function in a cohort of PN-dependent pediatric patients.A retrospective analysis studied 32 pediatric patients with a variety of medical diagnoses who received PN as a primary means of nutrition for 6 months or longer. Patients received variable proportions of their total caloric intake as PN, which ranged from 14%-100%. Iodine and thyroid function levels were obtained by serum sampling.No patient in our cohort of 32 demonstrated thyroid dysfunction or developed iodine deficiency. The length of time on PN and the percentage of total nutrition intake as PN were not associated with iodine levels (P < .89 and P < .73, respectively). There were no significant associations between age (P < .342), clinical diagnosis (P < .46), or sex (P < .43) on iodine status. There were no incidences of abnormal iodine levels in our cohort. Our study suggests that pediatric patients older than 6 months receiving PN may not benefit from iodine supplementation, but further investigation is needed.
View details for DOI 10.1177/0884533615611846
View details for PubMedID 26507189
- Intractable Diarrhea in Two Brothers: Late Diagnosis of Tufting Enteropathy in Adolescence.Digestive diseases and sciencesHaas, K., Martin, B., Martín, M., Kerner, J.2016; 61 (2): 381-383
- ACTG2 variants impair actin polymerization in sporadic Megacystis Microcolon Intestinal Hypoperistalsis SyndromeHUMAN MOLECULAR GENETICSHalim, D., Hofstra, R. W., Signorile, L., Verdijk, R. M., van der Werf, C. S., Sribudiani, Y., Brouwer, R. W., van IJcken, W. J., Dahl, N., Verheij, J. M., Baumann, C., Kerner, J., van Bever, Y., Galjart, N., Wijnen, R. H., Tibboel, D., Burns, A. J., Muller, F., Brooks, A. S., Alves, M. M.2016; 25 (3): 571–83
Abstract
Megacystis Microcolon Intestinal Hypoperistalsis Syndrome (MMIHS) is a rare congenital disorder, in which heterozygous missense variants in the Enteric Smooth Muscle actin γ-2 (ACTG2) gene have been recently identified. To investigate the mechanism by which ACTG2 variants lead to MMIHS, we screened a cohort of eleven MMIHS patients, eight sporadic and three familial cases, and performed immunohistochemistry, molecular modeling and molecular dynamics (MD) simulations, and in vitro assays. In all sporadic cases, a heterozygous missense variant in ACTG2 was identified. ACTG2 expression was detected in all intestinal layers where smooth muscle cells are present in different stages of human development. No histopathological abnormalities were found in the patients. Using molecular modeling and MD simulations, we predicted that ACTG2 variants lead to significant changes to the protein function. This was confirmed by in vitro studies, which showed that the identified variants not only impair ACTG2 polymerization, but also contribute to reduced cell contractility. Taken together, our results confirm the involvement of ACTG2 in sporadic MMIHS, and bring new insights to MMIHS pathogenesis.
View details for PubMedID 26647307
- Index of suspicion.Pediatrics in review Todd, S., Arora, R., Kannikeswaran, N., Allarakhia, I., Sivaswamy, L., Wallenstein, M. B., Burgener, E. B., Klotz, J., Kerner, J. A.2014; 35 (10): 439-446
- Hodgkin lymphoma following adalimumab for the treatment of Crohn's disease in an adolescent.Digestive diseases and sciencesRodriguez, A. A., Kerner, J., Luna-Fineman, S., Berry, G. J.2014; 59 (10): 2403-2405
- Hodgkin Lymphoma Following Adalimumab for the Treatment of Crohn's Disease in an AdolescentDIGESTIVE DISEASES AND SCIENCESRodriguez, A. A., Kerner, J., Luna-Fineman, S., Berry, G. J.2014; 59 (10): 2403-2405
- Case 3 Lactic Acidosis and Cardiovascular Collapse in a Teen With Ulcerative ColitisPEDIATRICS IN REVIEWWallenstein, M. B., Burgener, E. B., Klotz, J., Kerner, J. A.2014; 35 (10): 444–46
- Evaluation of Intestinal Biopsies for Pediatric Enteropathy A Proposed Immunohistochemical Panel ApproachAMERICAN JOURNAL OF SURGICAL PATHOLOGYMartin, B. A., Kerner, J. A., Hazard, F. K., Longacre, T. A.2014; 38 (10): 1387-1395
Abstract
Congenital enteropathies are rare disorders with significant clinical consequences; however, definitive diagnosis based on morphologic assessment of duodenal biopsies with routine stains alone is often impossible. To determine the role of immunohistochemistry (IHC) in the evaluation for microvillous inclusion disease, congenital tufting enteropathy (intestinal epithelial dysplasia), and enteroendocrine cell dysgenesis, a series of duodenal biopsies from 26 pediatric patients with chronic/intractable diarrhea was retrospectively reviewed. IHC stains for CD10, EpCAM, chromogranin, and villin were performed on all biopsies, and the results were correlated with hematoxylin and eosin and ultrastructural findings using electron microscopy, when available. Biopsies from 2 patients diagnosed with microvillous inclusion disease at the time of original biopsy demonstrated diffuse CD10-positive cytoplasmic inclusions within enterocytes and normal expression of EpCAM and chromogranin. Biopsies from 3 patients, including 2 siblings with confirmed EPCAM mutations, demonstrated complete loss of EpCAM expression and normal expression of CD10 and chromogranin; electron microscopic evaluation revealed characteristic ultrastructural findings of tufting enteropathy. Biopsies from 1 patient with a confirmed NEUROG3 mutation demonstrated an absence of intestinal enteroendocrine cells by chromogranin staining, consistent with enteroendocrine cell dysgenesis. Four patients' biopsies displayed nonspecific staining patterns for CD10 and/or EpCAM with normal expression of chromogranin, and 16 patients' biopsies exhibited normal expression for all 3 markers. Villin stains demonstrated heterogenous brush border labeling with nonspecific cytoplasmic reactivity, a pattern variably present throughout the biopsy series. In conclusion, the routine use of an IHC panel of CD10, EpCAM, and chromogranin is warranted in patients meeting specific age and/or clinical criteria, as the morphologic findings of congenital enteropathies may be subtle, focal, or inapparent on routine stains.
View details for Web of Science ID 000342001800010
- Misdiagnosis of Alpha-1 Antitrypsin Phenotype in an Infant with CMV Infection and Liver FailureDIGESTIVE DISEASES AND SCIENCESArias, P., Kerner, J., Christofferson, M., Berquist, W., Park, K. T.2014; 59 (8): 1710-1713
- Infliximab for the treatment of granulomatous peritonitis.Digestive diseases and sciencesYeh, A. M., Kerner, J., Hillard, P., Bass, D.2013; 58 (12): 3397-3399
- Multiple hepatic adenomas in a child with microvillus inclusion disease.Digestive diseases and sciencesBurgis, J. C., Pratt, C. A., Higgins, J. P., Kerner, J. A.2013; 58 (10): 2784-2788
- Evaluation of ethanol lock therapy in pediatric patients on long-term parenteral nutrition.Nutrition in clinical practice Pieroni, K. P., Nespor, C., Ng, M., Garcia, M., Hurwitz, M., Berquist, W. E., Kerner, J. A.2013; 28 (2): 226-231
Abstract
Pediatric home parenteral nutrition (PN) patients present a unique challenge with risks of catheter-associated bloodstream infections (CABSIs), sometimes requiring subsequent catheter removal. Recurrent infections can lead to line removal and potential loss of venous access in the future.Demonstrate that weekly ethanol lock therapy decreases CABSIs in long-term home PN patients and decreases line removals due to infections.Beginning August 2007, patients receiving PN with a history of multiple previous CABSIs were started on ethanol lock therapy. Seventy percent ethanol solution was instilled into the central venous catheter (CVC) for 2 hours weekly. Episodes of CABSIs and catheter removal due to infection were documented in patients prior to and after ethanol lock therapy.Fourteen patients were followed for an average of 690 days after ethanol lock therapy was initiated. These patients were found to average 9.8 CABSIs per 1000 catheter days prior to starting ethanol lock therapy and only 2.7 CABSIs per 1000 catheter days after ethanol lock therapy (P < .001). Prior to ethanol lock therapy, the group averaged 4.3 catheter removals per 1000 catheter days but only 1.0 catheter removal per 1000 catheter days after ethanol lock therapy.Our group of patients showed a 73% reduction in CABSIs and a 77% reduction in catheter removal due to infection after ethanol lock therapy. In our patient population, weekly ethanol lock therapy for 2 hours is an effective technique to reduce CABSIs and catheter removal in long-term home PN patients.
View details for DOI 10.1177/0884533612468009
View details for PubMedID 23232749
- ECHINOCANDIN AND ETHANOL LOCK THERAPY TREATMENT OF FUNGAL CATHETER INFECTIONSPEDIATRIC INFECTIOUS DISEASE JOURNALPieroni, K. P., Nespor, C., Poole, R. L., Kerner, J. A., Berquist, W. E.2013; 32 (3): 289-291
Abstract
Ethanol lock therapy has been implemented to prevent infections of central venous catheters as well as to treat infections. Fungal catheter-associated blood stream infections are historically more difficult to treat and have required removal of central venous catheters. We report the largest case series to date, successfully treating 5 of 7 fungal catheter-associated blood stream infections with ethanol lock therapy and systemic echinocandin administration.
View details for DOI 10.1097/INF.0b013e3182784867
View details for Web of Science ID 000314932700027
View details for PubMedID 23076381
- Aluminum Exposure in Neonatal Patients Using the Least Contaminated Parenteral Nutrition Solution ProductsNUTRIENTSPoole, R. L., Pieroni, K. P., Gaskari, S., Dixon, T., Kerner, J. A.2012; 4 (11): 1566-1574
Abstract
Aluminum (Al) is a contaminant in all parenteral nutrition (PN) solution component products. Manufacturers currently label these products with the maximum Al content at the time of expiry. We recently published data to establish the actual measured concentration of Al in PN solution products prior to being compounded in the clinical setting [1]. The investigation assessed quantitative Al content of all available products used in the formulation of PN solutions. The objective of this study was to assess the Al exposure in neonatal patients using the least contaminated PN solutions and determine if it is possible to meet the FDA “safe limit” of less than 5 μg/kg/day of Al. The measured concentrations from our previous study were analyzed and the least contaminated products were identified. These concentrations were entered into our PN software and the least possible Al exposure was determined. A significant decrease (41%–44%) in the Al exposure in neonatal patients can be achieved using the least contaminated products, but the FDA “safe limit” of less than 5 μg/kg/day of Al was not met. However, minimizing the Al exposure may decrease the likelihood of developing Al toxicity from PN.
View details for DOI 10.3390/nu4111566
View details for Web of Science ID 000311426800004
View details for PubMedID 23201834
View details for PubMedCentralID PMC3509507
- An Evolving Case of Concurrent Eosinophilic Esophagitis and Eosinophilic GastroenteritisDIGESTIVE DISEASES AND SCIENCESLe-Carlson, M., Triadafilopoulos, G., Pai, R. K., Kerner, J. A.2012; 57 (4): 842-844
- New advances in the management of children with intestinal failure.JPEN. Journal of parenteral and enteral nutritionPeterson, J., Kerner, J. A.2012; 36 (1): 36S-42S
- New Advances in the Management of Children With Intestinal FailureJOURNAL OF PARENTERAL AND ENTERAL NUTRITIONPeterson, J., Kerner, J. A.2012; 36: 36S-42S
- Chylous Ascites After Laparoscopic Nissen FundoplicationDIGESTIVE DISEASES AND SCIENCESPark, K. T., Adikibi, B., MacKinlay, G. A., Gillett, P. M., Sylvester, K. G., Kerner, J. A.2012; 57 (1): 28-31
- Immunophenotyping of Peripheral Eosinophils Demonstrates Activation in Eosinophilic EsophagitisJOURNAL OF PEDIATRIC GASTROENTEROLOGY AND NUTRITIONTammie Nguyen, T., Gernez, Y., Fuentebella, J., Patel, A., Tirouvanziam, R., Reshamwala, N., Bass, D., Berquist, W. E., Cox, K. L., Kerner, J. A., Nadeau, K. C.2011; 53 (1): 40-47
Abstract
Eosinophilic esophagitis (EoE) is a chronic inflammatory disorder characterized by upper gastrointestinal symptoms and the presence of high numbers of eosinophils in the esophagus. Although eosinophils in the esophagus have been found to be activated in subjects with EoE, detailed studies of intracellular signaling pathways involved in the mechanism of activation of eosinophils in EoE have heretofore been limited. The aim of the study was to assess whether any surface molecules or transcription factors are activated in peripheral eosinophils in subjects with EoE.Eosinophils and CD3+ lymphocytes were identified directly from 50 μL of whole blood of EoE and control subjects. Using Hi-FACS, levels of surface activation markers, including CD66b, and intracellular phosphoepitopes, including phosphorylated forms of signal transducer and activator of transcription (phospho-STAT) 1 and 6, were measured within each cell subset.Levels of surface CD66b as well as levels of intracellular phospho-STAT1 and phospho-STAT6 in peripheral blood eosinophils were significantly higher for untreated subjects with EoE vs healthy controls (P < 0.05). Levels of phospho-STAT1 and phospho-STAT6 in peripheral blood eosinophils were lower in subjects with EoE on therapy versus untreated subjects with EoE (P < 0.05).Levels of phospho-STAT1 and phospho-STAT6, transcription factors involved in inflammatory processes, were both significantly higher in peripheral eosinophils from untreated (ie, newly diagnosed) subjects with EoE versus subjects with EoE on therapy, healthy controls. Blood-based measurements of CD66b and phospho-STAT levels in peripheral eosinophils may be beneficial for identifying EoE.
View details for DOI 10.1097/MPG.0b013e318212647a
View details for Web of Science ID 000291925500006
View details for PubMedID 21694534
- Reversal of Hepatic and Renal Failure from Sickle Cell Intrahepatic CholestasisDIGESTIVE DISEASES AND SCIENCESKhan, M. A., Kerner, J. A.2011; 56 (6): 1634-1636
- The use of Omegaven in treating parenteral nutrition-associated liver diseaseJOURNAL OF PERINATOLOGYPark, K. T., NESPOR, C., Kerner, J.2011; 31: S57-S60
Abstract
Parenteral nutrition (PN), containing fat emulsions derived from soybean, has been implicated in the progression of PN-associated liver disease and cholestasis, particularly in infants with short bowel syndrome. Clinical use of Omegaven, a parenteral fish-oil emulsion, has been shown in recent studies to be a promising therapy to reverse liver disease and cholestasis. This review summarizes the rationale, relevant clinical investigations and future direction of Omegaven therapy for PN-dependent infants.
View details for DOI 10.1038/jp.2010.182
View details for Web of Science ID 000289236900009
View details for PubMedID 21448206
- Aluminum in pediatric parenteral nutrition products: measured versus labeled content.The journal of pediatric pharmacology and therapeutics : JPPT : the official journal of PPAGPoole, R. L., Pieroni, K. P., Gaskari, S., Dixon, T. K., Park, K., Kerner, J. A.2011; 16 (2): 92-97
Abstract
Aluminum is a contaminant in all parenteral nutrition solutions. Manufacturers currently label these products with the maximum aluminum content at the time of expiry, but there are no published data to establish the actual measured concentration of aluminum in parenteral nutrition solution products prior to being compounded in the clinical setting. This investigation assessed quantitative aluminum content of products commonly used in the formulation of parenteral nutrition solutions. The objective of this study is to determine the best products to be used when compounding parenteral nutrition solutions (i.e., those with the least amount of aluminum contamination).All products available in the United States from all manufacturers used in the production of parenteral nutrition solutions were identified and collected. Three lots were collected for each identified product. Samples were quantitatively analyzed by Mayo Laboratories. These measured concentrations were then compared to the manufacturers' labeled concentration.Large lot-to-lot and manufacturer-to-manufacturer differences were noted for all products. Measured aluminum concentrations were less than manufacturer-labeled values for all products.The actual aluminum concentrations of all the parenteral nutrition solutions were significantly less than the aluminum content based on manufacturers' labels. These findings indicate that 1) the manufacturers should label their products with actual aluminum content at the time of product release rather than at the time of expiry, 2) that there are manufacturers whose products provide significantly less aluminum contamination than others, and 3) pharmacists can select products with the lowest amounts of aluminum contamination and reduce the aluminum exposure in their patients.
View details for DOI 10.5863/1551-6776-16.2.92
View details for PubMedID 22477831
- Increased Number of Regulatory T Cells in Children With Eosinophilic EsophagitisJOURNAL OF PEDIATRIC GASTROENTEROLOGY AND NUTRITIONFuentebella, J., Patel, A., Nguyen, T., Sanjanwala, B., Berquist, W., Kerner, J. A., Bass, D., Cox, K., Hurwitz, M., Huang, J., Nguyen, C., Quiros, J. a., Nadeau, K.2010; 51 (3): 283-289
Abstract
There are limited data on the role of regulatory T cells (Treg) in the disease pathology of eosinophilic esophagitis (EoE). We tested the differences in Treg in subjects with EoE compared with those with gastroesophageal reflux disease (GERD) and healthy controls (HC).Pediatric patients evaluated by endoscopy were recruited for our study. Participants were categorized into 3 groups: EoE, GERD, and HC. RNA purified from esophageal biopsies were used for real-time quantitative polymerase chain reaction assays and tested for forkhead box P3 (FoxP3) mRNA expression. Treg were identified as CD4+CD25hiCD127lo cells in peripheral blood and as CD3+/FoxP3+cells in esophageal tissue.Forty-eight subjects were analyzed by real-time quantitative polymerase chain reaction: EoE (n = 33), GERD (n = 7), and HC (n = 8). FoxP3 expression was higher by up to 1.5-fold in the EoE group compared with the GERD and HC groups (P < 0.05). Protein levels of FoxP3 in blood and tissue were then investigated in 21 subjects: EoE (n = 10), GERD (n = 6), and HC (n = 5). The percentage of Treg and their subsets in peripheral blood were not significant between groups (P > 0.05). The amount of Treg in esophageal tissue was significantly greater in the EoE group (mean 10.7 CD3+/FoxP3+cells/high power field [HPF]) compared with the other groups (GERD, mean 1.7 CD3+/FoxP3+cells/HPF and HC, mean 1.6 CD3+/FoxP3+cells/HPF) (P < 0.05).We show that Treg are increased in esophageal tissue of EoE subjects compared with GERD and HC subjects. The present study illustrates another possible mechanism involved in EoE that implicates impairment of immune homeostasis.
View details for DOI 10.1097/MPG.0b013e3181e0817b
View details for PubMedID 20639775
- Increased HLA-DR Expression on Tissue Eosinophils in Eosinophilic EsophagitisJOURNAL OF PEDIATRIC GASTROENTEROLOGY AND NUTRITIONPatel, A. J., Fuentebella, J., Gernez, Y., Nguyen, T., Bass, D., Berquist, W., Cox, K., Sibley, E., Kerner, J., Nadeau, K.2010; 51 (3): 290-294
Abstract
The aim of the study was to investigate whether eosinophils have increased human leukocyte antigen (HLA)-DR expression in subjects with eosinophilic esophagitis (EoE) compared with controls.Patients who were undergoing an upper endoscopy with biopsies for suspected gastroesophageal reflux disease (GERD) or EoE at Lucile Packard Children's Hospital were enrolled. In total, the blood and tissue samples of 10 healthy controls (HC), 11 subjects with GERD, and 10 with EoE were studied. Multiple tissue staining to identify eosinophils (via eosinophil cationic protein-clone EG2) and major histocompatibility complex class II cell surface receptors (via HLA-DR) was performed via immunohistochemistry. The peripheral blood was analyzed using flow cytometry to detect eosinophil HLA-DR expression among these subjects.In the tissue, a greater proportion of eosinophils expressed HLA-DR among the subjects with EoE (mean 0.83 +/- 0.14, n = 9) relative to those with GERD (mean 0.18 +/- 0.19, n = 8, P < 0.01) and HC (mean 0.18 +/- 0.13, n = 6, P < 0.01). In total, 6 participants (4 HC subjects and 2 subjects with GERD) did not have any eosinophils identified on tissue staining and were unable to be included in the present statistical analysis. In the blood, there was no statistically significant difference in eosinophil HLA-DR expression among HC subjects (mean 415 +/- 217, n = 6), subjects with GERD (mean 507 +/- 429, n = 2), and those with EoE (mean 334 +/- 181, n = 6).These data demonstrate that the eosinophils from the esophagus of subjects with EoE have increased HLA-DR expression within this tissue.
View details for DOI 10.1097/MPG.0b013e3181e083e7
View details for Web of Science ID 000281453500008
View details for PubMedID 20639774
- Nickel Toxicity Presenting as Persistent Nausea and Abdominal PainDIGESTIVE DISEASES AND SCIENCESFuentebella, J., Kerner, J. A.2010; 55 (8): 2162-2164
- Aluminum Content of Parenteral Nutrition in Neonates: Measured Versus Calculated LevelsJOURNAL OF PEDIATRIC GASTROENTEROLOGY AND NUTRITIONPoole, R. L., Schiff, L., Hintz, S. R., Wong, A., Mackenzie, N., Kerner, J. A.2010; 50 (2): 208-211
Abstract
Aluminum (Al) is associated with significant central nervous system toxicity and bone and liver damage. Because Al is a contaminant of parenteral nutrition (PN) components including calcium and phosphate additives, premature infants are at potentially high risk for toxicity. The US Food and Drug Administration (FDA) has mandated PN component product labeling and recommended maximum Al daily exposure limits. The objective of this article is to determine the actual Al content of neonatal PN solutions, compare these values to the calculated amounts from manufacturers' PN product labels, and ascertain whether the actual Al exposure exceeds the FDA recommended maximum of 5 microg . kg(-1) . day(-1).Samples from 40 neonatal patient PN solutions were selected for sampling and Al content determination. Samples were also taken from 16 manufacturer's component products used in PN formulation. All of the samples were sent to Mayo Laboratories for Al content measurement. The calculated Al concentrations in PN samples were determined from the manufacturer's labeled content.Both measured and calculated Al concentrations exceeded the FDA recommended safe limit of
- Eotaxin and FGF enhance signaling through an extracellular signal-related kinase (ERK)-dependent pathway in the pathogenesis of Eosinophilic esophagitis.Allergy, asthma, and clinical immunology : official journal of the Canadian Society of Allergy and Clinical ImmunologyHuang, J. J., Joh, J. W., Fuentebella, J., Patel, A., Nguyen, T., Seki, S., Hoyte, L., Reshamwala, N., Nguyen, C., Quiros, A., Bass, D., Sibley, E., Berquist, W., Cox, K., Kerner, J., Nadeau, K. C.2010; 6 (1): 25-?
Abstract
Eosinophilic esophagitis (EoE) is characterized by the inflammation of the esophagus and the infiltration of eosinophils into the esophagus, leading to symptoms such as dysphagia and stricture formation. Systemic immune indicators like eotaxin and fibroblast growth factor were evaluated for possible synergistic pathological effects. Moreover, blood cells, local tissue, and plasma from EoE and control subjects were studied to determine if the localized disease was associated with a systemic effect that correlated with presence of EoE disease.Real-time polymerase chain reaction from peripheral blood mononuclear cells (PBMC), immunohistochemistry from local esophageal biopsies, fluid assays on plasma, and fluorescence-activated cell sorting on peripheral blood cells from subjects were used to study the systemic immune indicators in newly diagnosed EoE (n = 35), treated EoE (n = 9), Gastroesophageal reflux disease (GERD) (n = 8), ulcerative colitis (n = 5), Crohn's disease (n = 5), and healthy controls (n = 8).Of the transcripts tested for possible immune indicators, we found extracellular signal-regulated kinase (ERK), Bcl-2, bFGF (basic fibroblast growth factor), and eotaxin levels were highly upregulated in PBMC and associated with disease presence of EoE. Increased FGF detected by immunohistochemistry in esophageal tissues and in PBMC was correlated with low levels of pro-apoptotic factors (Fas, Caspase 8) in PBMC from EoE subjects. Plasma-derived bFGF was shown to be the most elevated and most specific in EoE subjects in comparison to healthy controls and disease control subjects.We describe for the first time a possible mechanism by which increased FGF is associated with inhibiting apoptosis in local esophageal tissues of EoE subjects as compared to controls. Eotaxin and FGF signaling pathways share activation through the ERK pathway; together, they could act to increase eosinophil activation and prolong the half-life of eosinophils in local tissues of the esophagus in EoE subjects.
View details for DOI 10.1186/1710-1492-6-25
View details for PubMedID 20815913
View details for PubMedCentralID PMC2976489
- Transcription Factors as Disease Indicators in Eosinophilic Esophagitis10th Annual Meeting of the Federation-of-Clinical-Immunology-SocietiesNguyen, T., Gernez, Y., Fuentella, J., Patel, A., Tirouvanziam, R., Reshamwala, N., Saper, V., Bass, D., Berquist, W., Kerner, J., Nadeau, K.ACADEMIC PRESS INC ELSEVIER SCIENCE.2010: S81–S82
- Liver Abscesses, Pylephlebitis, and Appendicitis in an Adolescent MaleDIGESTIVE DISEASES AND SCIENCESPatel, A. J., Ong, P. V., Higgins, J. P., Kerner, J. A.2009; 54 (12): 2546-2548
- Diversion Colitis in a 19-Year-Old Female with Megacystis-Microcolon-Intestinal Hypoperistalsis SyndromeDIGESTIVE DISEASES AND SCIENCESTalisetti, A., Longacre, T., Pai, R. K., Kerner, J.2009; 54 (11): 2338-2340
- Refeeding SyndromePEDIATRIC CLINICS OF NORTH AMERICAFuentebella, J., Kerner, J. A.2009; 56 (5): 1201-?
Abstract
Refeeding syndrome (RFS) is the result of aggressive enteral or parenteral feeding in a malnourished patient, with hypophosphatemia being the hallmark of this phenomenon. Other metabolic abnormalities, such as hypokalemia and hypomagnesemia, may also occur, along with sodium and fluid retention. The metabolic changes that occur in RFS can be severe enough to cause cardiorespiratory failure and death. This article reviews the pathophysiology, the clinical manifestations, and the management of RFS. The key to prevention is identifying patients at risk and being aware of the potential complications involved in rapidly reintroducing feeds to a malnourished patient.
View details for DOI 10.1016/j.pcl.2009.06.006
View details for Web of Science ID 000272846100011
View details for PubMedID 19931071
- Identifying Eosinophilic Esophagitis through Evaluation of Plasma Biomarkers65th Annual Meeting of the American-Academy-of-Allergy-Asthma-and-ImmunologyJoh, J., Huang, J., Nguyen, T., Vishwaanath, N., Patel, A., Fuentebella, J., Saper, V., Kerner, J., Cox, K., Berquist, W., Nadeau, K.MOSBY-ELSEVIER.2009: S169–S169
- Aluminum exposure from pediatric parenteral nutrition: Meeting the new FDA regulationJOURNAL OF PARENTERAL AND ENTERAL NUTRITIONPoole, R. L., Hintz, S. R., Mackenzie, N. I., Kerner, J. A.2008; 32 (3): 242-246
Abstract
Aluminum toxicity can cause serious central nervous system and bone toxicities. Aluminum is a contaminant of parenteral nutrition (PN) solution components. Premature neonates requiring high doses of calcium and phosphate to mineralize their bones, children with impaired renal function, and children on PN therapy for prolonged duration are at the highest risk. Effective in July 2004, the U.S. Food and Drug Administration (FDA) mandated labeling requirements for aluminum content in all PN solution components. To assess the aluminum exposure in neonatal and pediatric populations, this study aims to determine patients' daily aluminum load (mug/kg/d) delivered from PN solutions.The study included all inpatients who received PN during calendar year 2006 (13,384 PN patient days). The calculated parameters of mug/kg/d and mug/L of parentally administered aluminum were stratified according to patient age and weight. Aluminum content by product and manufacturer were tabulated.Forty-nine percent of the PN patient days were in patients weighing < 3 kg. These patients also received the largest amounts of aluminum (range, 30-60 mug/kg/d). Meeting the FDA regulation was possible only in patients weighing > 50 kg.Currently available parenteral products used to make PN solutions contain amounts of aluminum that make it impossible to meet the new FDA rule of
- Alteplase for the treatment of central venous catheter occlusion in children: Results of a prospective, open-label, single-arm study (The Cathflo Activase Pediatric Study)JOURNAL OF VASCULAR AND INTERVENTIONAL RADIOLOGYBlaney, M., Shen, V., Kerner, J. A., Jacobs, B. R., Gray, S., Armfield, J., Semba, C. P.2006; 17 (11): 1745-1751
Abstract
Alteplase is approved for use in the restoration of function to occluded central venous access devices (CVADs); however, there are few prospective studies in children. This study was undertaken to evaluate the safety and efficacy of alteplase in the treatment of CVAD occlusions in a pediatric population.A prospective, multicenter, open-label, single-arm study evaluating a maximum of two doses (< or =2 mg per dose) of alteplase was performed in pediatric patients. Inclusion criteria included patient age less than 17 years with an occluded CVAD (single-, double-, and triple-lumen catheter or implanted port). Patients with hemodialysis catheters, those with known mechanical occlusion, or those considered at high risk for bleeding or embolization were excluded. Assessment of function was made 30 and 120 minutes (if required) after each dose. The primary objective of the study was to evaluate the safety of alteplase as measured by the incidence of intracranial hemorrhage (ICH); secondary objectives included the evaluation of specific targeted serious adverse events and efficacy of alteplase in the restoration of catheter function.A total of 310 patients (174 male patients, 136 female patients; mean age, 7.2 years; range, 0.04-18.3 y) were treated; 55 of the patients (17.7%) were younger than 2 years of age. No patients experienced ICH (95% CI, 0%-1.2%). Nine serious adverse events were noted in eight patients (2.6% incidence), two of which were attributed by the investigator to study drug administration (one case of sepsis and one case of a ruptured catheter lumen). The cumulative rate of restoration of CVAD function after serial administration of a maximum of two instillations of alteplase, each with a maximum dwell time of 120 minutes, was 82.9% (95% CI, 78.2%-86.9%). Similar rates of catheter function restoration were seen among all catheter types studied; there were no clinically meaningful differences among age or sex subgroups.The administration of alteplase is safe and effective for the restoration of function to CVADs in pediatric patients.
View details for DOI 10.1097/01.RVI.0000241542.71063.83
View details for Web of Science ID 000242482400003
View details for PubMedID 17142704
- The use of IV fat in neonates.Nutrition in clinical practice Kerner, J. A., Poole, R. L.2006; 21 (4): 374-380
Abstract
IV fat emulsion (IVFE) is an integral part of the parenteral nutrition (PN) regimen in neonates. It provides a concentrated isotonic source of calories and prevents or reverses essential fatty acid deficiency. Continuous administration of IV fat with PN regimens prolongs the viability of peripheral IV lines in infants who might have limited venous access. IVFE must be administered separately from the PN solution in neonates. The acidic pH of a PN solution is necessary for maximum solubility of calcium and phosphorus. If fat emulsion is added to the PN solution, as is done in 3-in-1 (total nutrient admixture) solutions, the high amount of calcium and phosphorus needed by these infants may result in an unseen precipitate with serious consequences. Continuous fat infusion over 24 hours is the preferred method in neonates. The administration rate of 0.15 g/kg/hour for IVFE in the neonate should not be exceeded. Essential fatty acid deficiency can be prevented in neonates by providing IVFE in a dose of 0.5-1.0 g/kg/day. Carnitine is not routinely required to metabolize IVFE in the neonate. Infants should receive 20% lipid emulsion to improve clearance of triglycerides and cholesterol. Serum triglyceride levels should be maintained at
- Parenteral nutrition-associated cholestasis related to parental care.Nutrition in clinical practice Wu, P. A., Kerner, J. A., Berquist, W. E.2006; 21 (3): 291-295
Abstract
Parenteral nutrition-associated cholestasis (PNAC) is a complication not uncommon in the pediatric population. In severe cases, patients require a liver transplant. To our knowledge, we report the only case of PNAC with end-stage liver failure in a child with short bowel syndrome that resolved with a change in caretaker. Until his care was transferred from his abusive parents, he was frequently admitted for infection and sepsis. His liver function vastly improved from aspartate aminotransferase (AST) 3139 units/L, conjugated bilirubin 25.9 mg/dL to AST 47 units/L, direct bilirubin 0.3 mg/dL under the care of his attentive foster mother, and a liver transplant was no longer necessary. Bacterial infection and sepsis are risk factors correlated with patients with PNAC requiring liver transplant. Prevention of infection by a good caregiver may be a means to reduce the incidence of PNAC.
View details for PubMedID 16772546
- Hepatic infantile hemangioendothelioma with unusual manifestations16th Annual Meeting of the North-American-Society-of-Pediatric-Gastroenterology-Hepatology-and-NutritionBurtelow, M., Garcia, T., Lucile, S., Cox, K., Berquist, W., Kemer, J.LIPPINCOTT WILLIAMS & WILKINS.2006: 109–13
- Treatment of catheter occlusion in pediatric patientsConference on Evidence-Based Approach to Optimal Management of HPEN AccessKerner, J. A., Garcia-Careaga, M. G., Fisher, A. A., Poole, R. L.SAGE PUBLICATIONS INC.2006: S73–S81
Abstract
A proper initial assessment of catheter occlusion is the key to successful management. The assessment screens are for both thrombotic and nonthrombotic causes (including mechanical occlusion). If mechanical occlusion is excluded, thrombotic occlusion is treated with alteplase. Nonthrombotic occlusions are treated according to their primary etiologies: lipid occlusion is treated with 70% ethanol, mineral precipitates are treated with 0.1-N hydrochloric acid (HCl), drug precipitates are treated according to their pH-acidic drugs can be cleared with 0.1-N HCl, basic medications can be cleared with sodium bicarbonate or 0.1-N sodium hydroxide (NaOH). Prevention of occlusion of central venous access devices is also critical. To date, no data conclusively show heparin flushes to be superior to saline flushes. No prophylactic regimen, including low-dose warfarin, low-molecular-weight heparin, or 1 unit heparin/mL of parenteral nutrition has been endorsed by any major medical, nursing, or pharmacy group due to lack of scientific evidence. The most encouraging information on decreasing occlusion rate comes from experience with positive-pressure devices that attach to the hub of most catheter lumens and prevent retrograde blood flow and, consequently, decrease the risk of thrombus formation in the catheter lumen.
View details for Web of Science ID 000248557900013
View details for PubMedID 16387916
- Gastrointestinal manifestations of food allergies in pediatric patients.Nutrition in clinical practice Garcia-Careaga, M., Kerner, J. A.2005; 20 (5): 526-535
Abstract
Foods that account for 90% of allergic reactions in children are cow's milk protein, eggs, peanut, soy, tree nuts, fish, and wheat. Food allergy can manifest as urticaria/angioedema, anaphylaxis, atopic dermatitis, respiratory symptoms, or a gastrointestinal (GI) disorder. GI allergic manifestations can be classified as immunoglobulin E (IgE) mediated (immediate GI hypersensitivity and oral allergy syndrome); "mixed" GI allergy syndromes (involving some IgE components and some non-IgE or T-cell-mediated components) include eosinophilic esophagitis and eosinophilic gastroenteritis. Non-IgE-mediated or T-cell-mediated allergic GI disorders include dietary protein enteropathy, protein-induced enterocolitis, and proctitis. All these conditions share a common denominator: the response of the immune system to a specific protein leading to pathologic inflammatory changes in the GI tract. This immunological response can elicit symptoms such as diarrhea, vomiting, dysphagia, constipation, or GI blood loss, symptoms consistent with a GI disorder. The detection of food allergies can be accomplished by the use of radioallergosorbent (RAST) testing and skin prick tests in helping to assess the IgE-mediated disorders. Patch tests may help evaluate delayed hypersensitivity reactions. Treatment of GI allergic disorders ranges from strict dietary elimination of offending food(s), use of protein hydrolysates, and use of L-amino acid-based formula when protein hydrolysates fail. Treatment with topical (for eosinophilic esophagitis) or systemic steroids is used if all dietary measures are unsuccessful. Maternal breast feeding or the use from birth of hydrolysate formulas (extensive or partial hydrolysates) may be efficacious in the prevention of atopic disease in "high-risk" families (with at least 1 parent or sibling with a history of atopic disease).
View details for PubMedID 16207693
- Copper deficiency during parenteral nutrition: a report of four pediatric cases.Nutrition in clinical practice Hurwitz, M., Garcia, M. G., Poole, R. L., Kerner, J. A.2004; 19 (3): 305-308
Abstract
The standard of care for patients with cholestasis (direct bilirubin >or=2 mg/dL) while receiving parenteral nutrition (PN) solutions is to reduce or discontinue the copper and manganese. The repercussions of this action have not been studied. Two adult case reports document low serum copper levels associated with clinical symptoms of copper deficiency after the removal of copper from their PN solutions. We now describe the first known series of pediatric patients to develop copper deficiency after copper was removed from their PN solutions.
View details for PubMedID 16215119
- The use of alteplase for restoring patency to occluded central venous access devices in infants and children.Journal of infusion nursing : the official publication of the Infusion Nurses SocietyFisher, A. A., Deffenbaugh, C., Poole, R. L., Garcia, M., Kerner, J. A.2004; 27 (3): 171-174
Abstract
A 21-month retrospective review was completed at the Lucile Packard Children's Hospital to assess the experience of 22 infants and children who received alteplase for the clearance of occluded central venous access devices. After the first dose, 86% (n = 19) of the catheters cleared. Two additional catheters cleared with a second dose. With alteplase treatment, 95% (n = 21) of the catheters cleared. No adverse events were noted within 24 hours after the alteplase was received. Infusion of alteplase appeared to be safe and effective in restoring patency to occluded central venous access devices in infants and children.
View details for PubMedID 15118455
- A practical guideline for calculating parenteral nutrition cycles.Nutrition in clinical practice Longhurst, C., Naumovski, L., Garcia-Careaga, M., Kerner, J.2003; 18 (6): 517-520
Abstract
Both physiologic and psychological reasons for cycling total parenteral nutrition (TPN) have been well established. Despite widespread acceptance of this practice, the only previously published method for calculating TPN cycle rates is inherently flawed.A mathematical formula was derived to facilitate reliable calculation of cyclic TPN flow rates as a function of total volume and cycle time. A publicly accessible website was subsequently developed to expedite rapid determination of TPN cycles.A fail-safe method of calculating TPN cycle flow rates can be expressed as F = V/(4T-10), where F is equal to the basal flow rate (mL/h), T is equal to the desired cycle time (hours), and V is equal to the total volume of TPN (mL) to be delivered in 24 hours. The basal flow rate and twice the basal flow rate are used for the first and last 2 hours of the TPN cycle, and the remainder of the cycle runs at 4 times the basal flow rate. TPN cycles may be easily calculated online using this formula at http://peds.stanford.edu/tpn.html.We have developed a fail-safe method of calculating TPN cycle flow rates that will consistently deliver the desired volume and have made an online implementation of this formula publicly available.
View details for PubMedID 16215087
- A gastroenterologist's approach to failure to thrivePEDIATRIC ANNALS
新品、本物、当店在庫だから安心 新作新品モデル!グッドイヤー イーグル LSエグゼ 225/45R17 タイヤ通販 91W サマータイヤ GOODYEAR EAGLE 225/45R17 ミシュラン LS EXE




0-9 [A] BCDEFGHIJKLMNOPQRSTUVWXYZ [Index]
J v4.0a : s/n: softwar (No "e")
J. Graffman Calendar 2000 v2.9 Name: (Anything) s/n: EPOCH
J. Graffman Calendar 2000 v2.9.1 Name: (Anything) s/n: EPOCH
Jaba Com Web Browser v1.9.98 s/n: 0k7u0z6y1a981-3t6r3a5m7s24
Jaba Com Web Browser v1.9.99 s/n: 999-9999999999999999
Jack Hammer 2.1 name:RyDeR_H00k! Email: ryder@ucf.com id:1234-1234-1234-1234 s/n:BA91-7345-0000
JackHammer 1.5 : Order #: SAVAGE Regkey:78224938464138085318640458370445
Jackhammer User name:Xerox's CompuTerror Serial Number: 0BP2Z0VNDXAZ0C0476QY
JackHammer V2.2 Name: RyDeR_H00k! Email: ryder@ucf.com ID: 1234-1234-1234-1234 s/n: BA91-7345-0000
Jackpot Slots 1.5 : key:274955
Jackpot Slots 2.0 : key:274955
Jackpot Super Slots 1.55 name:Warezpup [KAC 99] password:182E43481723 code:5605F-05FB67910-169B3
Jackpot Super Slots v1.6.3 Name: Harlem Password: Niggah s/n: 2182E-82E434B34-3F265
Jacobs Image Browser V2.0.0 name:accz of blizzard code:4D2
Jacob's Math Training V2.0 Name: CDE 2001 Copies: 10000 s/n: 280544
Jam 98 MP3 Playlist Maker Name: SkorpyioN s/n: JAM98-022-C2A5104-000043210000-1C62BD0A
Jam 98 MP3 Playlist Maker V22 Name: SkorpyioN s/n: JAM98-022-C2A5104-000043210000-1C62BD0A
Jambient V0.9 Name: Amando Rodriguez s/n: 6221-B761-B580-046F
James Gleick's Chaos V1.01 s/n:900000-01101-05-0107
Jammer 2000 Name: Demian/TNT! s/n: 132000-JAMMER2000-35
Jammer 2000 V4.0 Name: William Clinton s/n: 180000-JAMMER2000-47
Jammer SongMaker : s/n: JWS11413
Jammer v1.9 s/n: 4w5tp96b
Jammer v1.95 Name: NaG3_TeaM s/n: 1122334-EB1605E627 or Name: Licensed User s/n: 1111111-0C1F2C17F3 or Name: Shaligar^Lash s/n: 1234567-2D503C3951
Jammer V2.0 s/n: 59956-E8C1CA010A
Jammer V2.0.0328 s/n: 0/VX2J+Fkv4f1A+VwWdNnvxQ2jFnDwkTZOzY2DwdQ9eAequTg/p/BkhpKUU5QGc5TLy6/fqR46YCEGXhr9nogg0ZUqLGWngr+Z3yq5HATPlIfURh4NEXkaIiXrzqZUs6L0KCGMVzFv1sAZCiV4Bz4rUtfrjXbTzQ+5LKpePAhOEA=
Jamming v2.6 s/n: HHH13141928
Jamming V2.9.1 Name: nowhereman s/n: ZK3A3141928
Janus GridEX 2000 V2.0 Name: aerosmith Company: FCN CDKey: JSGDX-95829-GPGHR-35882-89198 AuthCode: CA65FFFE
Janus GridEX Retail v1.6d : s/n: CSGDX-31255-YUKKM-12103-56422
Janus GridEX v1.6b s/n: CSGDX-31255-YUKKM-12103-56422
JarHelper V3.5.1 s/n:60035GE-AJ-314314
JAS 95 v1.4 : Name: Azrael [PC] s/n: CNK-atEa
Jasc Paint Shop Pro V7.01 s/n:G-1038M-DBT9M-N8KCL
Java Browser V2.1 name:forcekill company:infra code:454353453
Java Draw : name:Steve Hsu s/n:Rw|Ae_M}q
Java Embedded Server 1.0 : s/n:JS0876939287244113
Java Perk 4.0-4.1 code:1$3456189283
Java Safe 1.0 : s/n:JS 0243 8494 8708 4565
Java Script It V1.4 name:LOMAX company:DSI code:16@vh7ujs
Java Script it v1.5 : FirstName: LOMAX LastName: DSI s/n: 16@vh7ujs or FirstName: Skorpien LastName: TbC s/n: 1!z6;h?9@jjs
Java Script It V2.02 Name: independent s/n: 233838js or Name: CZYCZYCZY s/n: 238658js
Java Script It! V1.3 : First name:LOMAX Last name:DSI s/n:16@vh7ujs
Java Web Server V1.1.3 : s/n:JS2671414474923375
Java WorkShop v1.0 : s/n: JWS100-AT4072-888641479 or s/n: JWS100-CO6222-048623471 or s/n: JWS100-DA2082-879883481 or s/n: JWS100-DAAES4-906052896 or s/n: JWS100-DAAESU-906052896 or s/n: JWS100-IF2902-901345480 or s/n: JWS100-JS1212-119673481 or s/n: JWS100-KN4162-088731469 or
Java WorkShop v2.0 : s/n: JSW100-RV9797-929569987 or s/n: JWS100-DAAESU-906052896
JavaPC V1.1 s/n:JS8266699581686405
JavaScript Maker V2.7 s/n: soQty82gO
JavaScript Scrambler V1.1 name:LOMAX s/n:4438-716-8
Jaws PDF Creator V2.0 s/n: HFF0DETFIV2LNE0C
JayTrax V1.0 s/n:BOB-28701-FCJ
JayTrax V1.1b s/n:BOB-28701-FCJ
JayTrax v2.0 Name: Azrael [PC] s/n: 13956064
JBall V1.0 Name: Evidence Team s/n: 82606860
JBlurb Professional Edition V3.11 Code:104300000005-004
JBlurb V2.1 Pro s/n: 734502499634-103
JBlurb V3.0 Pro s/n: 104300000005-004 or Users: 31337 s/n: 303842031337-422 or Users: 999999 s/n: 736913999999-705
Jbuilder Pro v3.0 : s/n: 300-000-0071 Key: 9bx6-x0x0
JBuilder V5.0 Enterprise s/n: xa52-?npkv-gcqzw Key: m69-tet
JC ActiveDoc v1.0.1 : RegCode: Caleb Loring s/n: 712-a13fd0b4
JCanvas Studio Expert Edition V1.02 s/n: jcsv10-expert-23455345
JCheck v1.0 RC1 s/n: 2501-0000FF-9D
JCheck v1.20 s/n: 4809-0000DB-9F
JCheck v1.21 Beta 1 Name/Company: (Anything) s/n: 2501-0000FF-9D
JCheck v1.22 s/n: 4809-0000DB-9F
JChecker v1.0.3 Name: [k]rack Works s/n: 58514
JClass BWT 3.5 s/n:70035FS-QF-315151
JClass BWT v3.0 s/n: 75010FS-GP-314394
JClass Chart Bytecode v3.6j : s/n: 79036FS-KG-315563
JClass Chart v3.0 s/n: 79010FS-WB-314356
JClass Chart v3.5 s/n: 79035FS-JL-314748
JClass DataSource V3.5 s/n:87035FS-LJ-314038
JClass DataSource V3.5.1 s/n:87035FS-VY-314208
JClass Enterprise Suite v3.6.1 s/n: 62036GE-8V-314602
JClass Enterprise Suite V5.0.0K s/n: 63050GE-9B-346003
JClass Field Bytecode v3.6j : s/n: 83036FS-NS-315241
JClass Field v3.0 s/n: 83010FS-EY-314381
JClass Field v3.5 s/n: 83035FS-S7-314715
JClass HiGrid V3.5 s/n:85035FS-LS-314038
JClass HiGrid V3.5.1 s/n:85035FS-XV-314189
JClass JarHelper V3.5 s/n:79035FS-JL-314748
JClass JarMaster V4.5.1K s/n: 93045GE-EQ-343211
JClass LiveTable Bytecode v3.6j : s/n: 70036FS-VF-315802
JClass LiveTable v3.0 : s/n: 70030FS-BY-314675
JClass LiveTable v3.5 : s/n: 70035FS-QF-315151
JClass PageLayout v1.1.0 : s/n: 91011FS-PF-314084
JClass Standard Suite v3.5.1 : s/n: 60035GE-AJ-314314
JClass Swing Suite 1.1 : Bytecode:89011FS-S9-314018 Sourcecode:90011FS-JD-314016
JDBC Driver V2.20JC2 s/n: MET#A270999 Key: TYWOMF
JDTricks 2000 V1.2 Name: Ahlman s/n: 329E211
JDTricks 2000 V1.5 Name: Ahlman s/n: 329E211
JDTricks 2000 V1.5 Name: Ahlman s/n: 329E211 or Name: d-view s/n: 103B20F
JDTricks 2000 V1.51 Name: DiSTiNCT TEAM s/n: BA37A767D773A
JDTricks V2001 Name: Flesh Says [WPC] s/n: 77B3AD7593DAE8C3
Jedit v2.0 s/n: 65516
Jedit v2.0.5 s/n: 131053
Jedit v3.0 Name: [k]rack Works s/n: 363626484
Jedit v3.0.x Name: [k]rack Works s/n: 2815806861 or Name: Inpher s/n: 2697381898
Jeek v1.1 Name: tYruS@c4n.edu s/n: O4ICWO3G0XX07XOR
JeeKey CeDor V4.0b s/n: 340689
JellyFish v3 Name: Plushmm [PC97] s/n: 101313506404208
JellyFish32 v3 name:Plushmm [PC97] s/n:101313506404208
Jennifer vs Sarah 1.0 s/n:8JG-7NT-000521
Jeroboam v3.02 Name: [ORiON] - sixb0nes ][ s/n: xIGNAnPgdj
Jeroboam v3.03 Name: -=- ORiON -=- s/n: GIadvdhYFj
Jeroboam v3.04 s/n: GIadvdhYFj
Jeta Reyes For MAX 2.x name:Kashmir s/n:41025
Jeta Reyes v2.x Name: Kashmir s/n: 41025
JetAudio V4.92EX s/n: JADWB-F057-B3BC-78A1-1DEC
JetColor v1.20 Name: ZiuHu/TEX99 s/n: K6247982 or Name: Einhorn [Breakpoint] s/n: FB6257902
Jetforms Central v5.1 s/n: 1100-10479-6
Jetforms Design V5.1 s/n:1100-10479-6
Jetforms Transformation Builder v5.1 : s/n: 1100-10479-6
Jewl Linr V2.3 name:davy - blizzard s/n:NvEJvP7Cy5
JeWLinr V1.7 G-RoM 57aUKwYPO6 ZiLLY Pszz7wYPO6 PHRoZeN CReW ZRaU4hiQV6
JeWLinr V1.7 name:ZiLLY s/n:Pszz7wYPO6
JewlLinr V1.2 :Registered User :XzTZUyB3p8
JewlLinr V2.0 name:EzD s/n:7Ywa1wYPO6
JewlLinr v2.3 Name: davy - blizzard s/n: NvEJvP7Cy5
JewlLinr v2.4 Name: Matter of Darkness s/n: 7vGG3z7NsL
JFCSuite Enterprise V5.01 Password: stop Key: 7850-2100165-7450881
JFEdit Pro V3.24 s/n: AAFC-122X-IGSL
JFEdit V5.02 s/n: AAFC-122X-IGSL
JFEdit V5.04 s/n: AAFC-122X-IGSL
JForge v2.61 Key: steven anger Code: 6yCBtY89ox
JGO Screen Saver Wizard V2.1 Name: TUC PC2K s/n: 178-1160-16-160
Jigsaw-It v1.0 s/n: 7104400480 or s/n: 7101300271 or s/n: 7104401272
JigSoft v1.2g : s/n: 503-331
Jikia NetSpeed V3.0.450 Name: Mr.GReeN [WkT!] s/n: I1XN-1197-0542
JIM V1.0 s/n: 32253-CGE-26787 or s/n: 01617-IGR-55371
JimsQuest Woofpool 1999 Name: TUC PC99 s/n: 81378713
JimsQuest Woofpool v4.25 Name: Phrozen Crew s/n: 17718812
J-Kerner: s/n: T4K-10241-3CQ
JMP v3.1.6 s/n: 2611
JMP V4.x s/n: AD00009156
Job Track v5.4 s/n: house
JobLog V1.6.1 s/n: 385947305
JobLog V1.8 Name: Mac s/n: 125456289
JobTime V3.10 s/n: 9j3ciHf0wVJ
JobTrack v5.4e Name: Azrael [PC] s/n: house
JOC Downloader 1.2 beta name:MISTERE[INSIDE] s/n:5798544489
JOC Email Checker v1.20 Name: Dazzler s/n: 8501CR1737
JOC Web Promote V1.0 name:MISTERE[INSIDE] s/n:9798544499
JOC Web Promote v1.20 Name: Ringer s/n: 9774004827PSCO6299
JOC Web Promote v1.21 Name: MISTERE[INSIDE] s/n: 9798544499
JOC Web Spider V3.00 Name: MAGDAMARI CABIYA s/n: 77D21-A70F0CD-EE662
Joe's SmartProxy V1.0.2 Name: unknown s/n: 1819618497
Joggler V1.04 name:Audrey Jones Address: Brooklyn, NY 11234 email: slidah@hotmail.com RegNum: C1F 5451C145C1F492477
Joggler V1.06 name:jog [DNG] code:C1F 1A75145C1F378558
Joggler V1.06a name:Warp code:C1F-809145C1F376050
Joker Wild Video Poker V2.6 name:fungus / blizzard code:LLB6034
Joker Wild Video Poker V2.7 name:Warp code:DJM0416
Joker Wild Video Poker v2.75 Name: Warp s/n: DJM0416
Joker Wild Video Poker v3.0 Name: AEROSMITH s/n: EH0411A
Jones in the fast lane name:Gummy s/n:(leave blank)
Joshua's ChordTutor v1.52 s/n: NS-100-000-003 Key: AD3A-581B
Jot plus Notes 2.2.0 build 156 : name:dustie of blizzard s/n:1998 code:N9Z7BN6V1
Jot v2.0 : Name: bob bob s/n: 3455796966791929
Jot+ Notes 2.0.1 build 59 32bit : name:Fully Licensed User s/n:8937 code:19FH1GW0AQP
Jot+ Notes 2.1.1 name:Norway/Revolt98 s/n:1129 key:152A1BFJ14YI
Jot+ Notes 2.11 Build 134 name:BaMa/MANiFEST s/n:6666 code:G621E5JM2N
Jot+ Notes v2.0.1 build 59 Name: Fully Licensed User s/n: 8937 Code: 19FH1GW0AQP
Jot+ Notes v2.2.0 build 156 Name: dustie of blizzard s/n: 1998 Code: N9Z7BN6V1
Journal Safe 2001 V1.0.1 Name: LINDA HAGOOD s/n: ENF-1211-yo8Y-2114
Journal Safe 2001 V1.0.12 Name: LINDA HAGOOD s/n: ENF-1211-yo8Y-2114
Jova Konto V3.6.1 Name: NUKEM s/n: 4721694
jovaEinkauf V1.5 Name: nObOdy s/n: 50869317
JovaEinkauf V1.5.5 b Name: NUKEM/DBC s/n: 50869317
jovaSparbrief V2.1 Name: nObOdy s/n: 95322615
Joystick's Friend v1.0 Name: L!M!T / The Exterminators s/n: 11114115763377
JPad 3.1.3 build 99a : User id:10000000#400101 Keycode:808565617
JPad Pro v3.2 build 99a Name: 20000139#400101 s/n: 420631652
JPad Pro v3.7.297 Name: BaRT SiMPSoN s/n: 733253764
JPad Pro v3.7.305 Name: ArseniK of CORE s/n: 882345602
JPad v3.1.3 build 99a Name: 10000000#400101 s/n: 808565617
JPEG File Explorer v1.5 Name: CZY s/n: C-579-25362
JPEG Optimizer V1.32 s/n: JO1638
Jpeg Optimizer V2.00 s/n: qo7012
JPEG Optimizer V2.02 s/n: kj7246
JPEG Optimizer v3.03 s/n: FY9281
JPEG Optimizer v3.06 s/n: RW3418
JPEG Optimizer v3.07 s/n: AY8124 or s/n: WP8442
JPEG Optimizer v3.10 s/n: AY8124
JPEG Optimizer V3.15 s/n: JS$28921
JPEG Optimizer V4.00 s/n: JS$28921
JPEG Wizard v1.3 Name: `maIs s/n: 100637159 or Name: SATAN s/n: 104024119
JPEG Wizard V1.3.8 Name: Pookie s/n: 107415354
JPEG Wizard v1.31 Name: Mr.WhiTe [WkT!] s/n: 188222560
JPEG Wizard V1.4.0 Name: Nemesis] TNT s/n: 161732143
JPEGBatcher: s/n: RJPG-0147-OYuz
JpegDownLoader V1.0.3 s/n: 0103-2851-0005-2227
JpegDownLoader V1.x s/n: JKA55-05612-001
JpegDownLoader V2.0.1 s/n: 3190-9864-9076-3256
JPEmail V1.01 FirstName: Javier LastName: Villafane Company: Upskirts Inc s/n: XLM9 - PTQB - J161 - U126
J-Perk V4.2 : Hit Unlock/Register and enter: password:1$2876558201Jaba Com Web Browser 1.9.98 : s/n:0k7u0z6y1a981-3t6r3a5m7s24
J-Perk v5.01 s/n: 2$F48W6299T7 or s/n: 2$X48W6299T7
J-Perk V5.02 s/n: 2PX48W6299T7
J-Perk V5.2 s/n: 2PF48W6299T7
J-Perk V6.0 s/n: 2PF48W62T6T6
J-Perk V6.01 s/n: 2PF48W62T6T6
J-Perk V6.02 s/n: 2PF48W62T6T6
JPG Librarian and Veiwer v1.09 : Name: BSC s/n: 122288933996 or Name: Jaydee 99 s/n: 446264331297
JProbe Coverage Developer Edition v2.0 : s/n: 48020FS-WQ-314167
JProbe Coverage Professional Edition v2.0 : s/n: 49020FS-4N-314121
JProbe Developer Suite v2.5 s/n: 64PEERK-Y2-E2NR22
JProbe Developer Suite V2.8.1 s/n: 64PTFWK-MB-DT8R22
JProbe Developer Suite V3.0 s/n: 64P9QZK-BG-BX8Z22
JProbe Developer Suite V3.01 s/n: 64PHRZK-DS-BX8622
JProbe Profiler Developer Edition v2.0 : s/n: 40020FS-2V-315511
JProbe Profiler Professional Edition v2.0 : s/n: 41020FS-DB-314252
JProbe Profiler V1.1 s/n:40011FS-M9-314086
JProbe Profiler v1.1.1 s/n: 40011FS-M9-314086
JProbe ServerSide Suite v2.5 s/n: 65PZCRK-PJ-K2NR22
JProbe ServerSide Suite V2.8 Linux Server: 69PABRK-H2-N28R22
JProbe ServerSide Suite V2.8 Server: 65P79WK-MX-MULR22 Developer: 64PD3WK-EX-KT8R22
JProbe ServerSide Suite V2.8 Solaris s/n: 67PLTWK-NQ-NT8R22
JProbe ServerSide Suite V3.0 s/n: 65PY3JK-M8-SDR622
JProbe Threadalyzer Developer Edition v2.0 : s/n: 44020FS-CD-314174
JProbe Threadalyzer Professional Edition v2.0 : s/n: 45020FS-55-314120
JR Ware COMplete v2.0 s/n: 86911260
JR Ware COMplete v2.9 s/n: 86911260
JReversi V1.8 s/n: bwcxszjnev
JRS Multimedia Explorer v1.0 : s/n: IpX?MU23r!
JRun Pro v2.3 s/n: _MuFFiN_[uCF]-99999999-99-JSM.UL-1-0-5f37-154d
JRun Pro v2.3.3 s/n: JR23ULW-5104051005 or s/n: JR23PRW-5206251001
JRun Server V3.1 Enterprise s/n: JR300E1-0200-6270-1028
JS Office V1.2 Win95/NT : name:FALLEN s/n:666777666 Reg: 1BF5A492
JS Office V1.3 name:Versace Theking s/n:11002855 Reg: 57A6B0D3
JS Office V1.4 name:EinZtein s/n:9D3FE627 Reg: E0696352
JSB Surf Control for Proxy Server v2.61 : s/n: 0w1g001751lalxsaikh
JSB Surf Control Scout s/n: 0w1g001751lalxsaikh
JSB Surf Control Super Scout s/n: 0w1g001751lalxsaikh
JSentry Proxy Server for Linux v2.3 s/n: JALS080966U1024Z
JSentry Proxy Server v2.3 s/n: JALS08096651019
JShop Pro v2.0 s/n: 01184011631
JShop Pro v2.1a Name: (Anything) s/n: 01184011631
JShop Pro V3.03 Name: MFD Corp. s/n: JSP3X-7262040
JSMail v3.56.1556 s/n: C07463U00T00F4DBB436001800009A0200000405
JSource v1.1 s/n: Bark!-0001-0001-0002
jSQL v1.31 Name: jman s/n: N1HM1S
jSQL V1.4.1 Name: Pinnacle s/n: TYR26ZHZ7S
JStrip V2.0 Name: Andrenalin [GWA] s/n: 06-321324-801120-200836
JStrip V2.02.0026 Name: Predator [PC/pGC] s/n: 16-326118-401120-240689
JStrip V2.10 Name: fREaKaZoiD [lz0] s/n: 07-616977-921120-544965
JStrip V2.11 Name: IceWorld s/n: 06-423041-281119-995153
JSuite V5.0 Enterprise s/n: 7750-0200279-7371525 or s/n: 7799-8600719-2803212
JSuite V5.01 Enterprise Password: stop s/n: 7750-2100390-2835514
Jterm v2.0J s/n: JTRM-00217165
Jterm v3.0J s/n: JTRM-00351729 or s/n: JTRM-00309632
jtScroll V1.0.1 s/n: SCRL-3897291950891
JukeBytes V1.00.123 Name: TEAM ElilA s/n: 1143244000
JukeBytes V1.00.127 Name: aa s/n: 114018673 or Name: slushy s/n: 868060368
JukeBytes V1.2 Name/Company: Nemesis] TNT s/n: 1376489469
Jump Over V1.20.0210 Name/Town: TEAM ElilA s/n: 770026
Jump to Jump v1.10 : s/n: jtjs1009
Jumpers V1.1 s/n:JUMP4986
JumpOver V1.0.190 Name: TUC City: PC2K s/n: 474430-CA9-324
JumpOver V1.10.199 Name: Team ElilA Company: Team ElilA s/n: 775071-DCA-334
JumpOver V1.11.202 Name: Nemesis] City: TNT!Crack!Team s/n: 41036624
Jungo KernelDriver V5.02 Choose "Registered Version" Password for KernelDriver: 9d26ab7c Password for KernelDriver *SOURCES*: 9d341d0b Reboot if requested, when run WinDriver Wizard and enter: License: 68C9BECCEDE89D5060EF8FC5BD1BA552.Warlock//SSG
Jungo WinDriver V5.02 Choose "Registered Version" Password for WinDriver: a8dc72fe Reboot if requested, when run WinDriver Wizard and enter the following license: License: 68C9BECCEDE89D5060EF8FC5BD1BA552.Warlock//SSG
Just Add OS/2 Warp s/n: GDLIT224
Just between Friends v2.1 : s/n: epngdfho
Just Checking v1.8 s/n: 15386217
Just Checking V1.9.5.1 Name: BlazeBud [ORiON] s/n: 12341126
Just Checking V2.0 Name: Team ElilA s/n: 11168907
Just Checking V2.01 Name: TEAM ElilA s/n: 9178251 or Name: TeaM LAXiTY s/n: 9395925
Just Checking V2.02 Name: TeaM LAXiTY s/n: 9395925
Just Checking V2.10 Name: TeRMiNaToR [ACF] s/n: 2452241
Just Checking V2.12 Name: Evidence s/n: 11705055
Just Checking V2.13 Name: TEAM LAXiTY s/n: 7298803 or Name: ActMagO/TNT! crackers s/n: 6727345
Just Strategy's W32 Kriz Remover V1.0 Name: HAZARD s/n: hp6p1vd
Just The Fax v2.8 Name: Versus s/n: RKS-3388178 or Name: n03l s/n: RKS-1756575
Just The Fax v2.8b Name: Warp s/n: RKS-2180098
Just The Fax v2.8g Name: REKiEM / PCY '99 s/n: RKS-6116770
Just The Fax v2.8i Name: AzzYRiAN s/n: RKS-3858352
Just The Fax V2.9s Name: Raybiez Cracking s/n: RKS-7720601
Just The Fax V2.9u Name: RKS s/n: RKS-1666317
Just The Fax V2.9v Name: weed2k s/n: RKS-2508412
Just! Audio v1.0 : s/n: 01294-80802579s
Just! Audio V2.0 (build 1.92) : s/n:01246-99014884b
JustIn V2.3 s/n: B09WQ7R3TX72
Juuret V2.02.0072 Senior Name: KARHU s/n: D85-6795
Juxto V1.1 name:DSI code:459$9267
J-Write v2.4 Name: Ringer s/n: 7-007192
What’s New in the J-Kerner serial key or number?
Screen Shot
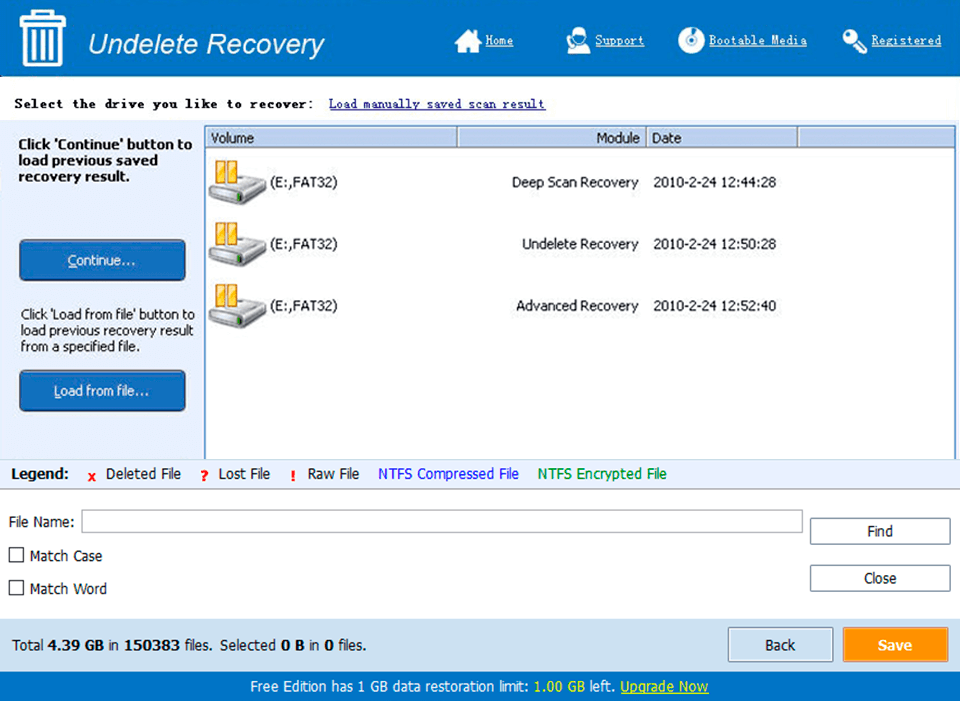
System Requirements for J-Kerner serial key or number
- First, download the J-Kerner serial key or number
-
You can download its setup from given links:


