
Mobile DB 1.31 serial key or number

Mobile DB 1.31 serial key or number
Homebrew Formulae
Health Information: What Can Mobile Phone Assessments Add?
by Margareta Warrén Stomberg, RNA, PhD; Birgitta Platon, RNA; Annette Widén, RN; Ingegerd Wallner, RN; and Ove Karlsson, MD
Abstract
In healthcare, pain assessment is a key factor in effectively treating postoperative pain and reducing the risk of developing chronic pain. The overall aim of this study was to investigate whether a mobile phone support system can be used as a basis to continuously document patients’ health information in real time and provide conditions for optimal, individual pain management after cholecystectomy and hysterectomy procedures.
In this pilot study, two randomly selected groups of patients provided information about their pain for one week postoperatively. One group responded via cell phones, and the other, a control group, responded using paper-based questionnaires.
The mobile phone system was found to provide a fast and safe basis for reporting pain postoperatively in real time. The results indicate that on days 3 and 4 the mobile phone group reported significantly higher levels of pain than the control group, and the cholecystectomy patients reported significantly more pain at movement on days 3 and 4 than the hysterectomy patients.
The mobile phone approach is an adaptation to modern technology and the mobility of individuals. This technology is user friendly and requires minimal support. However, as the sample size was small (n = 37), further studies are needed before additional conclusions can be drawn.
Keywords: mobile technology; pain management
Introduction
Today, the amount of surgery being performed on a day-surgery (outpatient) basis or using the enhanced recovery after surgery (ERAS) protocol is continuously increasing, which requires a well-established routine to follow up on pain and other symptoms postoperatively.1
Pain assessment is a key factor in successful pain management, and numerous studies show the necessity of treating postoperative pain effectively to reduce the risk of patients’ later developing chronic pain.2–6 Consequently, a prerequisite for optimal pain treatment is continuous pain assessment, also after discharge. Information that patients themselves provide is important in clinical research; however, collecting patient-reported survey data is a challenge.
One method of data collection available for almost all Swedes is mobile phones. Similarly, much of the worldwide population is also able to send and receive information this way. Thus, a flexible way of obtaining health information is through its documentation via patients’ own mobile phones. In this method, data from the mobile phone are directly transferred to a database available at the hospital, which gives the patient more freedom because a measured value can be entered whenever the patient chooses or it is requested. The method also enables professionals to adjust pain treatment immediately after receiving data from the patient, thus also giving staff a more individualized concept of how the pain develops throughout the day. This technique was tested in a pilot study, after which a more interactive and comprehensive study of this technology will be implemented in our postoperative recovery process.
Objectives
The primary aim of this study was to investigate whether a mobile phone support system can, in real time, provide a basis for obtaining continuous health information and provide conditions for optimal, individual pain management. The secondary aim was to evaluate a mobile computer system for capturing data (Medipal, Novatelligence AB, Stockholm, Sweden).
Methods
At random, an intervention group (using mobile phones to evaluate pain) and a control group (responding by questionnaires) were created. The questions regarding pain evaluation were the same for both groups and used a graded, numerical scale from 0 to 100. This pilot study was carried out from the spring of 2010 until January 2011 at a university hospital in Sweden.
Participants
Adult patients who understood the Swedish language in speech and writing and could manage their own mobile phones were invited to participate. Patients whose journal entries indicated alcohol and/or drug abuse or memory impairment were excluded. Forty relatively healthy patients ranging in age from 18 to 66 years were allocated from the surgical waiting list. Of these, 20 patients had been admitted for a planned vaginal hysterectomy and 20 for a laparoscopic cholecystectomy. After informed consent, during the preoperative stage, these patients were randomized to either the mobile phone group or the control group (Table 1 and Figure 1).
Mobile Phone Group
The patients in the mobile phone group were informed and thoroughly trained, preoperatively as well as prior to their discharge from the hospital, to document their pain levels on the mobile phone every four hours (from 8 a.m. to 8 p.m.). Furthermore, the participants in the mobile phone group and the charge nurses had access to technical support and written instructions during the study period. Additional assessments could be initiated by the patients at any time of the day.
Control Group
While these participants were given the same information regarding the pain evaluation questions as the mobile phone group, they were required to answer them on paper-based questionnaires every four hours for a period of four days after surgery. Additional pain assessments could be made on the questionnaires by the patients at any time of the day.
Procedure
The study began in the hospital the day of surgery. Prior to the study period, the software program was installed in the patients’ own mobile phones.
Each patient was given information individually and had the opportunity to test the application and provide test answers. The functionalities of the mobile phone, including how to move from question to question both forward and backward, as well as how to input a response and use the navigation keys, were carefully explained.
The follow-up of the mobile phone group was conducted by using a numeric rating scale from 0 to 100 (0 = no pain, 100 = terrible pain) with a mobile computer system, Medipal (Novatelligence AB, Stockholm, Sweden). After waking from the anesthesia, the patients’ mobile phones initiated pain measurements by a “push” function every four hours, for a period of six days following surgery. If the patient did not respond, a reminder in the form of an incoming Short Message Service (SMS) was sent once, after 13 minutes. The specified response time was a feature built into the program itself. Each question appeared separately in real time on the mobile phone screen and disappeared from the screen immediately after the response was given.
Communication was transferred between the handset and the company´s server via the mobile network GPRS, General Packet Radio Service. From the server, the encrypted health information was available to dedicated staff members in hospital.
The strong encryption used by this technology ensured the safe transfer of information through the system. All patient-related information that was sent from the mobile phone, whether iPhone, Android or Java was encrypted. In addition, only authorized users had access to patient information, and user names and passwords were required for access. If an incorrect password was entered three times, the service was blocked and could only be activated manually by an authorized technician at Novatelligence. All traffic between the web browser and website was encrypted with a certificate. Medipal’s servers and databases are hosted at www.interoute.com, which is not only ISO27001 certified but also holds data and records for some Swedish public healthcare providers. Furthermore, Medipal’s server has the same security and requirements as those prescribed for all medical record administration within Swedish public healthcare.
Patients were also able to report additional assessments between the specified time periods if they experienced especially painful episodes. All health information was incorporated into the patients’ health record. After six days, the nurse called the patient to remove the program from the mobile phone. At the same time, designated nurses asked structured questions that focused on potential difficulties in managing the mobile phone technology or in providing the daily responses to the questionnaires.
The control group received the follow-up questionnaire before surgery and was asked to reply to the questions at the same points in time as the mobile phone group, starting immediately after waking from the anesthesia. These questionnaires were returned in a prepaid envelope after the study period. No reminders were given to this group, which was followed up for four days postoperatively.
Analysis
The measured values for pain were compiled for the different time periods in each day. These values were subsequently analyzed for the two surgical procedures and the intervention and control groups. The mean level of measurements was calculated for each day. It was a requirement that a measurement could only be analyzed if the same participant responded correctly at all of the specified times of the days. If the response was incorrectly made, the value measured was not analyzed. All the additional measurements reported between the specified times, from both groups, were analyzed separately.
Mantel’s test was used to compare pain intensity between the surgical procedures and between the intervention and control groups. The amount of contact between the in-hospital care unit and the participants was documented, as was the patients’ need for technical support from Medipal.
Ethical Considerations
The clinic manager approved this pilot study, and after informed consent the patients were instructed on the technology. Their identity was encoded with a fictitious identifier when the data were transferred. In addition, the Medipal company ensured that no unauthorized person could access the data transfer.
Results
A total of 40 patients were allocated to the two groups; 20 used the mobile phone technology and 20 (the control group) answered the paper-based questionnaire. In all, 37 patients completed the survey. The response period began as soon as the patients were awake after surgery and continued for a period of six days for the mobile phone group and four days for the control group. The day of surgery was regarded as day 1 (see Table 1).
The response rate on the day of surgery (day 1) varied, resulting in 35 responses from the mobile phone group and 41 responses from the control group. No patient in the control group provided the responses completely for all of the specified times. When surgery was performed late in the afternoon, more responses were missed on that day. On days 2–4 postoperatively, the response rate was 100 percent, and no internal data were missing for either group. On days 5–6 the response rate was 69 percent for the mobile phone group; the control group was not required to answer the questionnaire on those days (see Figure 2).
As Figure 2 illustrates, no patient fully completed all the answers in the control group (paper-based questionnaires) on day 1, while one patient did so in the mobile phone group.
The cholecystectomy patients reported significantly more pain at movement on days 3–4 than the hysterectomy patients (p < .001). On days 3–4 the mobile phone group reported significantly higher pain levels.
Overall, additional pain assessments were made on 28 occasions in the mobile phone group, and none were made in the control group. These assessments showed that the average pain at rest was 65 (range 40–100) for all the participants, regardless of diagnosis, additional responses, and response method, and the average pain level at rest was about 40 (range 0–100) on days 1–4. Altogether, the pain level tended to be highest in the afternoon and evening.
Telephone Follow-up
After the sixth postoperative day, the patients were called to remove the program from their mobile phones and at the same time to evaluate the technology. When patients were asked to rank the difficulties in handling the mobile technology, from 1 to 10 (1 = no problem and 10 = very problematic), the mean value was 1.31, which indicates that the technology was not difficult to handle. Three patients requested technical support for a total of four times during the study period.
According to the patients, the technology was not time-consuming, and they were all willing to use the method again. Several of them, regardless of age, clearly expressed their preference for the mobile phone technology compared to answering the questionnaire.
The participants who responded using the paper questionnaires did not report any problems with the technique, although a few commented on the difficulty of remembering to make their reports at specific points of time. No one in the control group made any additional assessments.
Discussion
This study focused on methods for obtaining health information from patients after surgery. The results indicate big differences between the number of pain measurement levels received from patients using the mobile phone system and from those using the paper questionnaires. In addition, the assessed levels of pain were significantly higher from patients using the mobile phone method. There is hardly any reason to suppose that the mobile phone group experienced a higher level of pain, as both surgical procedures require pain medication, and both were included in the same number. An explanation for the difference, similar to reasons suggested by Dupont et al.,7 could be that an electronic system may provide an anonymous environment that is perceived as safer than paper questionnaires, thus eliciting more credible answers. This method can be considered especially valuable since private and sensitive questions had to be answered. Patients may thus have a higher level of confidence in the privacy of the method, which encourages responses.
This study also showed that no participant from the control group completed all the requested responses on the day of surgery (day 1), while one participant in the mobile phone group did respond at all of the specified times. Such a lack of response would be understandable if all the participants in the control group had undergone surgery later in the day and were therefore not strong enough to answer the paper questionnaire on that day, but this was not the case. According to Dupont, it can also be assumed that when each question appears separately on the mobile phone screen and disappears from it immediately after the response is made, the desire to respond is facilitated.8 Since each question appears separately on a screen, it may promote a more concentrated reflection on the individual issue, while a list of questions on paper could disrupt the patients’ focus on a single question. On the other hand, perhaps the patients simply felt more comfortable using the mobile phone.
Similar to our study, Matthew et al. found that when a comparison was made between a paper-based method and a digital method in a randomized, controlled clinical study, there were fewer missing data with the digital method, and it was preferred by 82.8 percent of the patients.9 Matthew et al. did not find any significant correlation between age and difficulty in using the digital method, and neither did we in this study.10
This study demonstrates that patients found the mobile phone system convenient to use and that it was not a time-consuming method. A technology-based reminder to assess pain in real time provides valuable information compared with paper-based surveys that might be answered later, thus requiring the patient to recall the degree of pain that occurred some time ago. Similarly, Kristjansdottir found that although the participants were required to answer questions through a digital system several times a day, it was a user-friendly method.11
The development of such technology for sending and receiving different kinds of health-related information is at the forefront of quick and secure information exchange. Electronic methods for individual, patient-reported assessments not only add value over paper-based surveys, but they are also becoming more acceptable and are perceived as providing a greater degree of confidentiality. When the participants were randomized into the groups, most of them were interested in the mobile phone system, and some expressed disappointment on being allocated to the control group. Although some of the older mobile phones were unable to function with the Medipal program, causing a delay, most of the older mobile phones were upgraded with the support of Medipal. Nevertheless, a few participants were excluded since it was not possible to upgrade their mobile phones.
As home-based healthcare increases, including, for example, ambulatory surgery, so-called fast track surgery, and ERAS, the communication between patients and caregivers needs to be improved.12 The ongoing self-monitoring of pain and other symptoms by mobile phone appears to be an optimal method that meets the challenge of following several vital signs in real time.
This method enables caregivers to ensure patient safety and provide optimal access to care through regular mobile interaction with the patient. Another development will include smartphone applications for the patients. Rosser and Ecclestonfound that mobile phone applications can be used for pain education.13 In addition, this mobile technology has been found to be a good distraction technique. A randomized, controlled study demonstrated that anxiety was significantly reduced in the distraction technique group 45 minutes after operation, compared to the control group.14
Limitations and Areas for Further Study
The small number of participants, which is the main limitation of the study, prevents us from drawing any established conclusions from analysis of the pain levels. A further significant disadvantage was not carrying out the follow-up period for the same number of days for both groups. Additional study is thus necessary.
A further development of this pilot study would be to provide feedback to the patient by sending appropriate, individual information in real time, for example, details about changing the dosage of analgesic and improving any symptom control at home. Adequate symptom control can capture pain variations during the day and describe pain patterns over time as the patient moves about in the normal daily environment.
Conclusion and Clinical Implications
In this study, it was found that the mobile phone system provided a safe method with which to measure pain postoperatively in real time. On days 3–4 the mobile group reported significantly higher levels of pain than the control group (p < .001). Furthermore, only the mobile phone group reported additional pain measurements. Patients found the technique easy to use and were willing to use it again.
This project is an adaptation to modern technology and the mobility of individuals. As the use of mobile phones is expected to increase in the coming years and as their screen size and usability improves, there is reason to employ this technology more frequently in healthcare, which also helps the patient to stay mobile. The technology will improve clinical efficiency and care coordination.15
Significant advantages of the mobile phone method for surveys are the real-time measured outcomes, which are assumed to provide credible, monitored answers of different variables. This real-time information also facilitates communication between patients and caregivers, which enables them to make rapid decisions about individual treatment and improve health information.
Acknowledgments
We are grateful to Anna Cederlund and Marcus Smedman for their help.
Margareta Warrén Stomberg, RNA, PhD, is a senior lecturer and associate professor in health sciences at the University of Gothenburg/Sahlgrenska Academy and Sahlgrenska University Hospital/Östra in Gothenburg, Sweden.
Birgitta Platon, RNA, is a registered nurse anesthetist in the acute pain team in the gynecology and obstetrics department at Sahlgrenska University Hospital/Östra in Gothenburg, Sweden.
Annette Widén, CCRN, is a critical care nurse in the acute pain team at Sahlgrenska University Hospital/Östra in Gothenburg, Sweden.
Ingegerd Wallner, CCRN, is a critical care nurse in the acute pain team at Sahlgrenska University Hospital/Östra in Gothenburg, Sweden.
Ove Karlsson, MD, is a physician in the anesthesia department at the women’s hospital of Sahlgrenska University Hospital/Östra in Gothenburg, Sweden.
Notes
1. Segerdahl, M., M. Warrén Stomberg, N. Rawal, M. Brattwall, and J. Jakobsson. “Clinical Practice and Routines for Day Surgery in Sweden: Results from a Nation-wide Survey.” Acta Anaesthesiologica Scandinavica 52, no. 1 (2008): 117–24.
2. Gartner, R., M. B. Jensen, J. Nielsen, M. Ewertz, N. Kroman, and H. Kehlet. “Prevalence of and Factors Associated with Persistent Pain Following Breast Cancer Surgery.” Journal of the American Medical Association 302, no. 18 (2009): 1985–92.
3. Kehlet, H., T. S. Jensen, and C. J. Woolf. “Persistent Postsurgical Pain: Risk Factors and Prevention.” Lancet 367, no. 9522 (2006): 1618–25.
4. Kehlet, H., and J. P. Rathmell. “Persistent Postsurgical Pain: The Path Forward through Better Design of Clinical Studies.” Anesthesiology 112, no. 3 (2010): 514–15.
5. White, P. F., and H. Kehlet. “Improving Postoperative Pain Management: What Are the Unresolved Issues?” Anesthesiology 112, no. 1 (2010): 220–25.
6. Russ, A. J., L. D. Faucher, D. B. Gordon, T. A. Pellino, and M. J. Schurr. “Functional Implications of Long-Term Pain Following Outpatient Inguinal Herniorrhaphy—a Prospective Evaluation.” Journal of Surgical Research 169, no. 1 (2011): 25–30.
7. Dupont, A., J. Wheeler, J. E. Herndon II, A. Coan, S. Y. Zafar, L. Hood, M. Patwardhan, H. S. Shaw, H. K. Lyerly, and A. P. Abernethy. “Use of Tablet Personal Computers for Sensitive Patient-Reported Information.” Journal of Supportive Oncology 7, no. 3 (2009): 91–97.
8. Ibid.
9. Matthew, A. G., K. L. Currie, J. Irvine, P. Ritvo, D. Santa Mina, L. Jamnicky, R. Nam, and J. Trachtenberg. “Serial Personal Digital Assistant Data Capture of Health-Related Quality of Life: A Randomized Controlled Trial in a Prostate Cancer Clinic.” Health and Quality of Life Outcomes 5 (2007): 38.
10. Ibid.
11. Kristjansdottir, O. B., E. A. Fors, E. Eide, A. Finset, S. van Dulmen, S. H. Wigers, and H. Eide. “Written Online Situational Feedback via Mobile Phone to Support Self-Management of Chronic Widespread Pain: A Usability Study of a Web-based Intervention.” BMC Musculoskeletal Disorders 12 (2011): 51.
12. Adamina, M., H. Kehlet, G. A. Tomlinson, A. J. Senagore, and C. P. Delaney. “Enhanced Recovery Pathways Optimize Health Outcomes and Resource Utilization: A Meta-analysis of Randomized Controlled Trials in Colorectal Surgery.” Surgery 149, no. 6 (2011): 830–40.
13. Rosser, B. A., and C. Eccleston. “Smartphone Applications for Pain Management.” Journal of Telemedicine and Telecare 17, no. 6 (2011): 308–12.
14. Mosso, J. L., A. Gorini, G. De La Cerda, T. Obrador, A. Almazan, D. Mosso, J. J. Nieto, and G. Riva. “Virtual Reality on Mobile Phones to Reduce Anxiety in Outpatient Surgery.” Studies in Health Technology and Informatics 142 (2009): 195–200.
15. Putzer, G., and Y. S. Park. “Are Physicians Likely to Adopt Emerging Mobile Technologies? Attitudes and Innovation Factors Affecting Smartphone Use in the Southeastern United States.” Perspectives in Health Information Management (Spring 2012): 1–22.
Printer friendly version of this article.
Margareta Warrén Stomberg, RNA, PhD; Birgitta Platon, RNA; Annette Widén, RN; Ingegerd Wallner, RN; and Ove Karlsson, MD. “Health Information: What Can Mobile Phone Assessments Add?” Perspectives in Health Information Management (Fall 2012): 1-10.
Gb. gzip. id. in.
.What’s New in the Mobile DB 1.31 serial key or number?
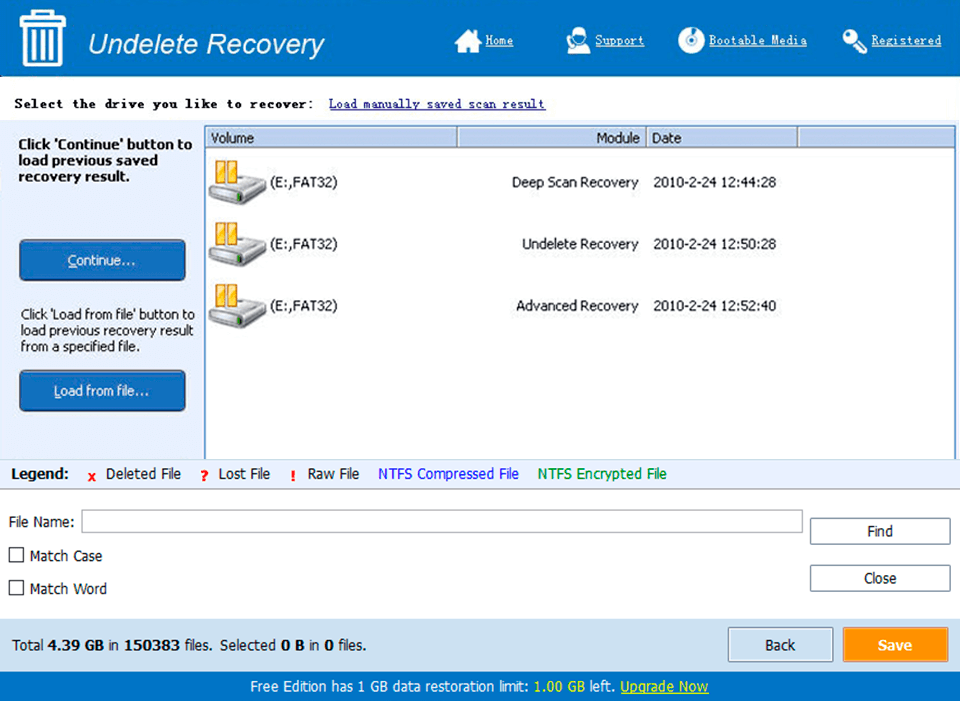
Screen Shot
System Requirements for Mobile DB 1.31 serial key or number
- First, download the Mobile DB 1.31 serial key or number
-
You can download its setup from given links:


