
Coronavirus serial key or number

Coronavirus serial key or number
Emerging COVID-19 success story: Germany’s strong enabling environment
Introduction
Throughout the COVID-19 pandemic, Germany has shown several elements of success across the four phases of our preparedness and response framework: prevent, detect, contain, and treat. The country’s incredibly strong enabling environment, including a good local public and health care system and expert scientific institutions, has largely contributed to this broad-based progress.
Germany did not prevent the COVID-19 outbreak, but the prevention protocols in place facilitated the country’s response to the outbreak. These protocols included early establishment of testing capacities, high levels of testing (in the European Union, Germany is a leader in tests per confirmed case), an effective containment strategy among older people (which may explain why Germany has a much lower case fatality rate than comparable countries), and efficient use of the country’s ample hospital capacity.
Prevent: Local health authorities, the Robert Koch Institute (RKI) – Germany’s public health institute – and other scientific institutions have produced data and analysis to inform Germany’s response. RKI and scientists at other institutions mobilized in early January to launch national crisis management to understand the epidemiology of the pandemic.
Detect: One of the first diagnostic tests for COVID-19 was developed at Berlin’s Charité hospital, and the government worked to mobilize the country’s public and private laboratories to rapidly scale up testing capacity. Later, Germany became a pioneer in polymerase chain reaction (PCR) testing, which continues to feature prominently in the national strategy.
Contain: Germany’s greatest success in this area has been relatively limited transmission in long-term care facilities. Because older people are more likely than younger people to die from the virus, the country is at higher risk because of its older population. The comparable low rate of infection among Germany’s population over age 70 is probably one driver of its relatively low case fatality rate overall.
Treat: With a large number of hospital beds and careful planning, Germany’s intensive care units (ICUs) have not been overly stressed, although health care workers have had to contend with shortages of personal protective equipment (PPE).
In April, Germany began relaxing its physical distancing measures, a strategy driven by data and science. This approach is informed by continuous tracking of key indicators and will be supplemented by findings from serological testing. A month after Germany began to relax physical distancing, the disease has shown few signs of resurging.
Context
Germany has the fourth largest economy in the world and spends approximately 11 percent of its gross domestic product on health care, with US$5,119 spent per capita per year.1,2 As a result, the capacity of Germany’s health care system is considered to be very high. In the European Union (EU), Germany has the most hospital beds per 1,000 people (8.3)3 and a robust sector of private and public laboratories, of which nearly 200 indicate capacity for SARS-CoV-2-tesing.4 It also ranks among the top five countries in the European Union for the number of nurses (13.2) and physicians (4.2) per 1,000 people.5
Germany has traditionally held the most restriction-free and consumer-oriented health care system in Europe.6 Health insurance is mandatory for all citizens and permanent residents of Germany, with approximately 90 percent of the population covered through nonprofit nongovernmental insurance funds and around 10 percent of the population covered through private insurance. In a Commonwealth Fund survey, Germany has the lowest wait times for both consultations with specialists and elective surgeries.7
The user-friendliness of the health care system and its ample human resources and physical infrastructure have led to exceptional and continuously improving health indicators. For example, life expectancy at birth grew from 75 years in 1990 to 81 years in 2018,8 and the maternal mortality ratio also decreased from 11 deaths per 100,000 live births in 1990 to 7 in 2017.9
The first case in Germany was reported on January 27in Bavaria. On February 1, the government further clarified reporting obligations and mandated that all health care providers report suspected cases of COVID-19 within 24 hours to local public health authorities.10 On February 27, with a total of 26 confirmed cases, the government set up an inter-ministerial national crisis management group. The next day, the government required all travelers entering the country from high-risk areas (such as, at that time, areas in China or Italy) to provide information about possible previous exposure and contact details.11 Testing is available at no cost to the patient upon medical or epidemiological indication and testing for epidemiological indications was also recently included in asymptomatic contacts or screenings. RKI began issuing daily situation reports for the national and international public health sector on January 23, although the first reports were confidential due to the granularity of the data.
Risk assessments and technical guidelines for testing, case finding, contact tracing, hygiene, and disease management, as well as various other documents, have been available since January 16. At the end of February and beginning of March, mass gatherings and travel were increasingly restricted. On March 10, mass gatherings with more than 1,000 participants were prohibited. In mid-March the federal states started to close schools. On March 18, non-EU citizens were barred from entering the European Union for 30 days.12 On March 22, Chancellor Angela Merkel announced that the federal states and national government had jointly decided to implement a “contact ban,” limiting public gatherings to two people (outside families), requiring physical distance of at least approximately 5 feet (1.5 meters), and closing many businesses. The contact ban was not a lockdown: The population remained free to leave the house, such as for walks. On April 10, all travelers arriving in Germany, regardless of their origin, were required to quarantine for 14 days.
All of these measures paid off. By April 15, when new cases reported per day numbered approximately 2,000 (compared to a peak in March of 6,000), the government announced a gradual easing of physical distancing measures. Thus far, the relaxation of these physical distancing measures has not caused an increase in new infections. On May 22, there were 460 new infections, indicating that Germany’s contact tracing and robust testing and treatment strategies may have brought the country through the most severe portion of the outbreak.
Prevent
Epidemiological expertise and surveillance
The German government entered the pandemic with a detailed National Pandemic Plan.13 Together with generic preparedness plans and other disease-specific plans and documents (e.g., for MERS), this detailed response plan enabled the government to activate quickly, with no time wasted on disputes related to governance, accounting, or costs.14
Because Germany is a highly federalized country, the responsibility for public health lies primarily with intermediate and local public health authorities in 16 federal states and approximately 400 counties. They adapt the national guidelines and recommendations to local needs. National authorities facilitate nationwide exchange and negotiate standards and common procedures.
As Germany’s national public health institute, RKI is dedicated to the prevention, control, and investigation of infectious diseases. In addition to routine surveillance, its team of scientists conducts research on infectious disease pathogenesis, risk assessment, epidemiology, and sentinel surveillance systems to support the federal government, local and intermediate public health authorities, and health professionals during outbreaks.15 RKI publishes risk assessments, strategy documents, response plans, daily surveillance reports on COVID-19, and technical guidelines, and works with national and international public health authorities as channels for distributing communication. This steady flow of information has helped the government—as well as local and intermediate public health authorities, health professionals, and the population—make critical decisions during the outbreak.
Detect
In January 2020, scientists at Germany’s Charité hospital developed one of the first specific tests for the presence of the SARS-CoV-2 virus in patients, which is now used widely around the world.16 The World Health Organization adopted it as one of the core diagnostic tests. Given how quickly the test was developed, Germany was able to turn its attention early to growing its testing capacity.17 The country was uniquely positioned to do this because its laboratories have the expertise, accreditation, and equipment to conduct PCR assays and quickly deliver diagnoses. On February 28, the government facilitated this process by mandating that all insurance companies pay for COVID-19 tests,18 incentivizing private laboratories to scale up quickly. On May 14, Germany extended this law to include testing of asymptomatic people to expand testing of at-risk groups who may have come in contact with COVID-19 patients, especially health care workers and those in nursing homes.19 As of May 11, 2020, Germany has conducted 18.6 tests per positive case, more than Italy (11.9), Spain (8.4), United States (7), United Kingdom (6.4), and France (6.3), but less than South Korea (68.1).20
Bavarian health authorities and scientists closely examined—and eventually broke—the chain of transmission among the first cluster of cases, which occurred at the end of January in Bavaria. Breaking this initial chain bought Germany critical time to design its response while yielding important lessons about how the disease is transmitted.21 By using a combination of epidemiological methods such as interviews and whole genome sequencing, the team was able to reconstruct and describe transmission events precisely. This research provided details on attack rates, incubation periods, and the serial interval, which provided critical information that enabled public health experts to estimate the potential size of the epidemic and decide on appropriate containment measures.22
Even when the number of cases grew exponentially in Germany, local public health and intermediate and national authorities continued to make tremendous efforts to conduct contact tracing for every single case, despite a lack of staff. Citizen science projects were launched to complement the government’s efforts: RKI released the Corona-Datenspende (Corona Data Donation) smartwatch app on April 7. The app works by collecting activity and heart rate data, along with postal codes, and analyzing the information for potential COVID-19 symptoms.23 The app is voluntary, and the collected information is currently being analyzed. In addition, RKI analyzes the aggregated and anonymized data of mobile phones to identify changes in the mobility of citizens.
Transmission chain of COVID-19 satellite outbreak in Bavaria, Germany, in January–February, 202024
The government also planned to develop a centralized contact tracing app that would enable health authorities to alert others who may have come into contact with people who were confirmed positive. After pushback due to privacy concerns, Germany decided to adopt a decentralized, anonymous approach to contact warning. It will work by asking individuals to report their positive test status via the app, and Bluetooth connections between phones trigger alerts to people who had come into contact with someone who tested positive.25 This app is also voluntary, so its effectiveness will depend on how many people download it and whether infected patients report their positive test status.
The biggest need related to contact tracing is human resources at local public health facilities, many of which are understaffed. The German Federal Ministry of Health and RKI hired and trained “containment scouts”— typically medical students—to support local authorities in tracing contacts.26 Health leaders emphasize the fundamental importance of contact tracing and need to maintain staff levels to keep caseloads low, so that contract tracers can keep up with the volume. Following up with all contacts becomes more difficult during larger outbreaks, regardless of the level of contact.
German scientists from the University of Bonn conducted some of the world’s first COVID-19 antibody studies in the hard-hit town of Gangelt, where it found community infection rates of nearly 14 percent.27 Among other scientific institutions planning serological studies, as part of its long-term strategy, RKI has announced a three-pronged approach to gathering data about community spread, with the idea that the data will help shape more sensitive policies in the future. The elements of its approach are:
- Serological examination of blood donors: Starting in April 2020, 5,000 blood samples from adults will be examined every 14 days to learn what percentage have antibodies present.
- Serological examination of COVID-19 hot spots in Germany: A representative sample of approximately 2,000 volunteers who are over 18 years and living in harder-hit areas within Germany will be examined several times. These volunteers will also be asked questions about clinical symptoms, previous illness, health behavior, living conditions, and mental health. This study started in mid-April 2020.
- Nationwide population representative screening: 15,000 people over the age of 18 are being examined at 150 study locations around the country. These people are meant to be a representative sample of the country.28
Contain
The first major international satellite outbreak outside of China happened in Germany at the end of January. A single index case from China hit Bavaria, a well-equipped region, but the local and regional resources for contact tracing were still immediately stretched.29 On February 1, 2020, the first flight of mainly German citizens returning from Wuhan arrived at Frankfurt Int’l Airport. PCR tests were carried out on all passengers to detect the presence of SARS-CoV-2, and two passengers were discovered to be positive. It was possible to prevent secondary cases, but cytopathic effects showed that both asymptomatic patients could have been contagious.30
These experiences may have increased awareness among health professionals and the public, so when several larger outbreaks began spreading a month later, information and technical guidelines were available and the public and politicians were alert.
On March 22, Germany enforced strict physical distancing guidelines, banning groups of more than two people in public and shutting down some businesses. Unlike many other EU countries, however, Germany never issued a curfew.
The average age of German citizens is 46, putting them at higher risk of complications from COVID-19 than younger populations; the average age of COVID-19 patients is 49.31,32 Germany’s case fatality rate among patients over 70 is the same as in most European Union countries (20.5 percent, compared with 18.9 percent in Spain and 19.5 percent in Italy).33,34 However, Germany has been able to limit the number of infections of people older than 70.Of Germany’s total number of cases, 19 percent are older than 70, compared with 36 percent in Spain and 39 percent in Italy. As a result, overall case fatality rates in Germany as of May 2020 are 4.6 percent, compared with 14.1 percent and 12 percent in Italy and Spain, respectively.35 South Korea has fared similarly to Germany by managing to keep infections among the over-70 population to only 11 percent of all cases, reporting a case fatality rate of 17 percent for this group, and maintaining a low overall case fatality rate of 2.4 percent.36 These data seem to indicate that quality of care for older patients does not vary widely among countries, but the success of containment among high-risk populations does.
In Germany the first outbreaks affected travelers, festivals, and workplaces, not nursing homes, which may have helped limit infections among older people. Eventually, there were more outbreaks among older people, but the majority of cases occurred in other settings.37 Germany has also been able to manage infection rates in hospitals and long-term care facilities. According to RKI national guidelines, recovered COVID-19 cases who return into care homes from hospitals must have tested negative or have undergone quarantine at an isolation area for 14 days.38 Furthermore, specific guidance is provided to nursing homes on hygiene measures and protocols to handle suspected and confirmed cases as well as outbreaks.39 Older people were also tested more often than younger age groups.
As of May, 37 percent of all deaths in Germany occurred in people who were cared for or accommodated in facilities such as facilities for the care of older, disabled, or other persons in need of care, homeless shelters, community facilities for asylum-seekers, repatriates and refugees as well as other mass accommodation and prisons. However, the percentage is much higher in several neighboring countries: 51 percent in Belgium, 66 percent in France, 61 percent in Norway, 66 percent in Spain, and 50 percent in Sweden.40
Treat
In March a register of ICUs was established by the German Interdisciplinary Association for Intensive Care and Emergency Medicine and RKI.41 Since April 16, ICU capacity and COVID-19 patients treated in ICU have been reported daily. These data help to understand the severity of the disease and potential impacts on the health care system. Based on daily reports showing a long-term trend of sufficient ICU capacity, the government passed a law on May 14 providing free ICU care to patients from other EU countries.42
The management of supplies of PPE has not been as successful. The government launched a crisis team to centrally procure PPE,43 and on March 4 it banned the export of all PPE.44 Despite these measures, Germany has seen shortages of more than 100 million single-use masks, 50 million filter masks, and 60 million aprons and disposable gloves, leading to a protest by health care providers on April 27.45 German authorities continue to work on procuring these supplies, but like many other countries around the world, they have yet to entirely solve the problem.
Conclusion
Germany’s strong health care system and early progress on detection complemented its effective containment strategy. Ensuring the increase of human resources among understaffed local public health facilities was another key component to enable more efficient contact tracing, but these resources may not be sustainable. Overall, Germany’s focus on collecting and analyzing data and communicating the results to the public is leading to an informed set of policy choices that is generating unusual levels of public support. Germany’s federal system has led to varied approaches and guidance from each state in distancing measures and subsequent loosening measures as well as greater capacity in the health system as a product of redundancies.
As of May, Germany is moving forward with relaxing its physical distancing guidelines but is doing so based on a data-driven rationale. Chancellor Angela Merkel regularly cites RKI surveillance data and uses epidemiological concepts such as reproduction rate as a driving factor behind decisions related to social distancing measures.46 The German government is focusing on three indicators—infection rate, disease severity, and health system capacity—to measure the quality of its response. Setting clear expectations and providing transparency to the public on the criteria for government decision making about reopening is a key factor in gaining public trust.
Immediately after relaxing measures, Germany saw a slight uptick in the virus reproduction rate47 but has been able to identify outbreaks in nursing homes and slaughterhouses to stop transmission. Germany has been successful in limiting the extent of its outbreak early on, but the key question over the coming months is whether it can prevent a second wave of infections while allowing greater freedom of movement.
Germany: Outbreak and Policy Action Timeline
In-depth explainers on Exemplar countries
Endnotes
World Bank. GDP (current US$) – Germany [data set]. World Bank Data. Washington, DC: World Bank. https://data.worldbank.org/indicator/NY.GDP.MKTP.CD?locations=DE&view=chart. Accessed June 1, 2020.
Tikkanen R, Osborn R, Mossialos E, Djordjevic A, Wharton GA. International Health Care System Profiles – Germany. The Commonwealth Fund. June 5, 2020. https://international.commonwealthfund.org/countries/germany/. Accessed June 6, 2020.
World Bank. Hospital beds (per 1,000 people) – Germany [data set]. World Bank Data. Washington, DC: World Bank. https://data.worldbank.org/indicator/SH.MED.BEDS.ZS?locations=DE&most_recent_value_desc=true. Accessed June 5, 2020.
Germany excels among its European peers. The Economist. April 25, 2020. https://www.economist.com/europe/2020/04/25/germany-excels-among-its-european-peers. Accessed June 1, 2020.
World Bank. Physicians (per 1,000 people) – Germany [data set]. World Bank Data. Washington, DC: World Bank. https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=DE&most_recent_value_desc=true. Accessed June 1, 2020.
Björnberg A. Euro Health Consumer Index 2018. Marseillan, France: Health Consumer Powerhouse; 2018. https://healthpowerhouse.com/media/EHCI-2018/EHCI-2018-report.pdf. Accessed June 1, 2020.
The Commonwealth Fund. 2010 Commonwealth Fund International Health Policy Survey. https://www.commonwealthfund.org/publications/surveys/2010/nov/2010-commonwealth-fund-international-health-policy-survey. New York: The Commonwealth Fund; 2010.
World Bank. Life expectancy at birth, total (years) – Germany [data set]. World Bank Data. Washington, DC: World Bank. https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=DE&name_desc=true. Accessed June 2, 2020.
United Nations Maternal Mortality Estimation Inter-Agency Group. Maternal Mortality in 2000-2017: Internationally Comparable MMR Estimates—Germany. Geneva: World Health Organization; 2019. https://www.who.int/gho/maternal_health/countries/deu.pdf?ua=1. Accessed June 1, 2020.
Empfehlungen des Robert Koch-Instituts zur Meldung von Verdachtsfällen von COVID-19 [Recommendations from the Robert Koch Institute for reporting suspected cases of COVID-19]. Robert Koch Institute website. Last updated May 29, 2020. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Empfehlung_Meldung.html. Accessed June 5, 2020.
Coronavirus SARS-CoV-2: Chronik der bisherigen Maßnahmen [Coronavirus SARS-CoV-2: Chronology of measures taken]. German Federal Ministry of Health. https://www.bundesgesundheitsministerium.de/en/coronavirus/chronologie-coronavirus.html. Accessed June 5, 2020.
Coronavirus Disease 2019 (COVID-19) Daily Situation Report of the Robert Koch Institute. April 3, 2020. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-03-04-en.pdf?__blob=publicationFile. Accessed June 2, 2020.
Robert Koch Institut. Ergänzung zum Nationalen Pandemieplan – COVID-19 – neuartige Coronaviruserkrankung [Supplement to the National Pandemic Plan – COVID-19 – Novel Coronavirus Disease]. Berlin: Robert Koch Institute; 2020. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Ergaenzung_Pandemieplan_Covid.html. Accessed June 8, 2020.
Eckner C. How Germany has managed to perform so many Covid-19 tests. The Spectator. April 6, 2020. https://www.spectator.co.uk/article/how-germany-has-managed-to-perform-so-many-covid-19-tests. Accessed June 1, 2020.
What we do – Departments and units at the Robert Koch Institute. Robert Koch Institute website. https://www.rki.de/EN/Content/Institute/DepartmentsUnits/DepartmentsUnits_node.html. Accessed June 5, 2020.
Researchers develop first diagnostic test for novel coronavirus in China. [Press release]. Charite. January 16, 2020. https://www.charite.de/en/service/press_reports/artikel/detail/researchers_develop_first_diagnostic_test_for_novel_coronavirus_in_china/. Accessed June 1, 2020.
Eckner C. How Germany has managed to perform so many Covid-19 tests. The Spectator. April 6, 2020. https://www.spectator.co.uk/article/how-germany-has-managed-to-perform-so-many-covid-19-tests. Accessed June 5, 2020.
Information on testing. Zusammen gegen Corona website. https://www.zusammengegencorona.de/en/inform/information-on-testing/. Accessed June 5, 2020.
Zweites Gesetz zum Schutz der Bevölkerung bei einer epidemischen Lage von nationaler Tragweite [Second law to protect the population in an epidemic situation of national scope]. German Federal Ministry of Health. https://www.bundesgesundheitsministerium.de/en/covid-19-bevoelkerungsschutz-2.html. Accessed June 2, 2020.
Hasell J, Mathieu E, Beltekian D, et al. Coronavirus (COVID-19) Testing. https://ourworldindata.org/coronavirus-testing. Accessed June 7, 2020.
Carrel P, Poltz J. It was the saltshaker: How Germany meticulously traced its coronavirus outbreak. The World Economic Forum COVID Action Platform. April 12, 2020. https://www.weforum.org/agenda/2020/04/it-was-the-saltshaker-how-germany-meticulously-traced-its-coronavirus-outbreak. Accessed June 1, 2020.
Böhmer MM, Buchholz U, Corman VM, et al. Investigation of a COVID-19 outbreak in Germany resulting from a single travel-associated primary case: a case series. Lancet Infectious Disease. 2020;S1473-3099(20)30314-5. http://doi.org/10.1016/S1473-3099(20)30314-5. Accessed June 5, 2020.
Einblicke in die Analysen der Corona-Datenspende [Insights into the analysis of corona data donation]. Corona-Datenspende website. https://corona-datenspende.de/. Accessed June 5, 2020.
Böhmer MM, Buchholz U, Corman VM, et al. Investigation of a COVID-19 outbreak in Germany resulting from a single travel-associated primary case: a case series. Lancet Infectious Disease. 2020;S1473-3099(20)30314-5. http://doi.org/10.1016/S1473-3099(20)30314-5. Accessed June 5, 2020.
Busvine D, Rinke A. Germany flips to Apple-Google approach on smartphone contact tracing. Reuters. April 26, 2020. https://www.reuters.com/article/us-health-coronavirus-europe-tech/germany-flips-on-smartphone-contact-tracing-backs-apple-and-google-idUSKCN22807J. Accessed June 1, 2020.
Beaumont P, Connolly K. Covid-19 track and trace: what can UK learn from countries that got it right? The Guardian. May 21, 2020. https://www.theguardian.com/world/2020/may/21/covid-19-track-and-trace-what-can-uk-learn-from-countries-got-it-right. Accessed June 1, 2020.
Regalado A. Blood tests show 14% of people are now immune to covid-19 in one town in Germany. MIT Technology Review. April 9, 2020. https://www.technologyreview.com/2020/04/09/999015/blood-tests-show-15-of-people-are-now-immune-to-covid-19-in-one-town-in-germany/. Accessed June 2, 2020.
Wie viele Menschen sind immun gegen das neue Coronavirus? Robert Koch-Institut startet bundesweite Antikörper-Studien. [How many people are immune to the new corona virus? Robert Koch Institute starts nationwide antibody studies]. [Press release]. Robert Koch Institute. https://www.rki.de/DE/Content/Service/Presse/Pressemitteilungen/2020/05_2020.html. Accessed June 5, 2020.
Böhmer MM, Buchholz U, Corman VM, et al. Investigation of a COVID-19 outbreak in Germany resulting from a single travel-associated primary case: a case series. Lancet Infectious Disease. 2020;S1473-3099(20)30314-5. http://doi.org10.1016/S1473-3099(20)30314-5. Accessed June 5, 2020.
Hoehl S, Rabenau H, Ciesek S et al. Evidence of SARS-CoV-2 Infection in Returning Travelers from Wuhan, China. N Engl J Med 2020; 382:1278-1280. https://www.nejm.org/doi/full/10.1056/NEJMc2001899. Accessed June 8, 2020.
Plecher H. Median age of the population in Germany 1950-2050. Statista website. April 8 2020. https://www.statista.com/statistics/624303/average-age-of-the-population-in-germany/. Accessed June 5, 2020.
Coronavirus Disease 2019 (COVID-19) Daily Situation Report of the Robert Koch Institute. May 16, 2020. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-05-16-en.pdf?__blob=publicationFile. Accessed June 5, 2020.
Coronavirus Disease 2019 (COVID-19) Daily Situation Report of the Robert Koch Institute. May 17, 2020. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-05-17-en.pdf?__blob=publicationFile. Accessed June 1, 2020.
Roser M, Ritchie H, Ortiz-Ospina E, Hasell J. Mortality Risk of COVID-19. Our World in Data website. https://ourworldindata.org/mortality-risk-covid?country=ESP+DEU+USA+ITA+KOR. Accessed June 5, 2020.
Roser M, Ritchie H, Ortiz-Ospina E, Hasell J. Mortality Risk of COVID-19. Our World in Data website. https://ourworldindata.org/mortality-risk-covid?country=ESP+DEU+USA+ITA+KOR. Accessed June 1, 2020.
Domestic occurrence status: Coronavirus Infection-19 Outbreak Status in Korea. Korean Ministry of Health and Welfare website. http://ncov.mohw.go.kr/bdBoardList_Real.do?brdId=1&brdGubun=11&ncvContSeq=&contSeq=&board_id=&gubun=. Accessed June 8, 2020.
COVID-19 (Coronavirus SARS-CoV-2). Robert Koch Institute website. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/nCoV.html. Accessed June 5, 2020.
COVID-19: Kriterien zur Entlassung aus dem Krankenhaus bzw. aus der häuslichen Isolierung [COVID-19: Criteria for discharge from hospital or from home isolation]. Robert Koch Institute website. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Entlassmanagement.html?nn=13490888. Accessed June 5, 2020.
Robert Koch Institute. Prävention und Management von COVID-19 in Altenund Pflegeeinrichtungen und Einrichtungen für Menschen mit Beeinträchtigungen und Behinderungen [Prevention and management of COVID-19 in elder care facilities and facilities for people with impairments and disabilities]. Berlin: Robert Koch Institute; 2020. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Alten_Pflegeeinrichtung_Empfehlung.pdf?__blob=publicationFile. Accessed June 5, 2020.
European Centre for Disease Prevention and Control (ECDC). Surveillance of COVID-19 in Long-Term Care Facilities in the EU/EEA, 19 May 2020. Stockholm: ECDC; 2020. https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-long-term-care-facilities-surveillance-guidance.pdf. Accessed June 2, 2020.
DIVI-Intensivregister website. https://www.intensivregister.de/#/index. Accessed June 5, 2020.
Coronavirus SARS-CoV-2: Chronik der bisherigen Maßnahmen [Coronavirus SARS-CoV-2: Chronology of measures taken]. German Federal Ministry of Health. https://www.bundesgesundheitsministerium.de/en/coronavirus/chronologie-coronavirus.html. Accessed June 5, 2020.
Coronavirus SARS-CoV-2: Chronik der bisherigen Maßnahmen [Coronavirus SARS-CoV-2: Chronology of measures taken]. German Federal Ministry of Health. https://www.bundesgesundheitsministerium.de/en/coronavirus/chronologie-coronavirus.html. Accessed June 8, 2020.
Coronavirus SARS-CoV-2: Chronik der bisherigen Maßnahmen [Coronavirus SARS-CoV-2: Chronology of measures taken]. German Federal Ministry of Health. https://www.bundesgesundheitsministerium.de/en/coronavirus/chronologie-coronavirus.html. Accessed June 8, 2020.
Connolly K. German doctors pose naked in protest at PPE shortages. The Guardian. April 27, 2020. https://www.theguardian.com/world/2020/apr/27/german-doctors-pose-naked-in-protest-at-ppe-shortages. Accessed June 2, 2020.
The Editorial Board. Germany’s new coronavirus thinking. The Wall Street Journal. May 14, 2020. https://www.wsj.com/articles/germanys-new-coronavirus-thinking-11589498695. Accessed June 2, 2020.
Coronavirus: Germany not alarmed by infection rate rise. BBC. May 12, 2020. https://www.bbc.com/news/world-europe-52632369. Accessed June 2, 2020.
Reuse our work freely
You can use all of what you find here for your own research or writing. We license all charts under Creative Commons BY.
All of our charts can be embedded in any site.
One coronavirus number will let us know if Australia's outbreak is getting worse
Updated August 18, 2020 14:27:40
With new daily coronavirus infections approaching the highest seen in Australia, the confidence many were starting to feel has been crushed by the outbreak in Victoria and growing clusters in NSW.
So with things changing quickly, is there a good way to track how Australia is doing that isn't so overwhelming?
Helpfully, there's one number that can tell us quickly and clearly whether the coronavirus outbreak is getting better or worse. It's called the growth factor.
The main thing to understand is this — to be sure we're getting the outbreak under control, we must get this number below one and keep it there.
And here is how the growth factor for Australia's outbreak currently looks.
What is 'growth factor' and why is it important?
Put simply, the growth factor measures how fast the number of new cases is going up or down.
And here's the key point:
- If the growth factor is above one, the number of new cases each day is going up. If it stays above one consistently, alarm bells should be ringing.
- If it's below one, we're getting (or keeping) the outbreak under control.
Calculating the daily growth factor is as simple as taking today's new reported cases and dividing it by yesterday's new cases. Because these numbers can be a little volatile we're calculating a daily growth factor based on a comparison of the past week's new cases to the week before.
Of course, the growth factor will change over time and even though Australia has had early success, the fight against coronavirus is likely to be a long one, as the current resurgence in Victoria highlights.
Even when the number of people sick with COVID-19 gets quite low, the virus can start spreading quickly again without ongoing vigilance.
Should I be worried when it goes above one?
Catherine Bennett, the chair of epidemiology at Deakin University, says how to interpret growth factor changes depending on how many new cases we're currently seeing.
When a country's outbreak is generally under control and we start seeing a fairly low number of new cases, "the importance of this number is really as a signal that something's changed over the last seven days and what we expect that to be now [in Australia] is probably clusters of cases."
When we see the growth factor go above one, we need to consider the details of the specific cases that pushed it up.
"When it's above one, it means that we've got work to do — we've got to make sure that the reason it's above one is well under control," Professor Bennett explains.
"I think it'll go above one really easily if we go and find another little cluster, and so that's something people have to be prepared for."
[Want to see how Australia's growth factor compares to the US, the UK and other countries around the world? Keep reading, or skip ahead.]
So while a growth factor briefly above one isn't necessarily cause for immediate alarm in Australia, it is worth being alert to, and there are a couple of scenarios which would make it more worrying.
The first is if it stays above one for too long.
The rapid spread of cases in Victoria illustrates this point perfectly — while the number of new cases started low, the growth factor has stayed above 1 for a month.
That's a full month where, on average, the number of new cases one day was higher than the day before.
While how far it is above one is important (this indicates more rapid growth), the nature of the spread of the virus means a few cases can turn into a crisis in weeks.
The second main reason to worry is the type of cases.
If lots of the cases being found are of an unknown origin — that is they're not traced to an existing case or imported as people continue to return from overseas — it indicates that there may be more disease circulating in the community than authorities are aware of.
What else should I know?
A figure like this is only ever as good as the data being collected. So when reading the growth factor, another important factor to keep in mind is testing.
It's possible more cases will be found in the community simply through the expansion of testing.
Professor Bennett notes that there is a correlation between the number of tests conducted and the number of new cases being found. However, she is also quick to point out that this correlation doesn't imply cause and effect.
"It could be you're doing a bit more testing, because you've discovered a case associated with [for example] an aged care facility, and then you go and screen everybody. So it could actually be linked to a specific case that triggered a bit more testing, but also it could just be that every time we look harder, we just pick up those extra few," she said.
Finally, it's worth remembering that even though the growth factor is a great litmus test for how well we're keeping Australia's outbreak in check, other numbers are important too.
Is growth factor the same as reproduction rate?
You might have heard state and territory medical officers or epidemiologists use terms like 'R', 'R0' or 'reproduction rate'.
Like growth factor, these are measures of how quickly a virus spreads through a community, however they are slightly different and the difference can be important.
Growth factor is a direct measure of the change in new cases being reported.
Reproduction rate is an estimate of how many new people will be infected, on average, by each person who has a disease. The most relevant measure is effective reproduction rate, sometimes referred to as Reff.
This is the estimated reproduction rate at a given point in time, taking into account the various control measures, like physical distancing, that are in place.
Estimates of reproduction rate are just that, estimates. They're based on modelling which takes a number of factors into account and often involves assumptions. These estimates can be very useful for epidemiologists and health authorities, however experts can often disagree about the true number.
How are other countries doing?
Now that we understand what growth factor means, it can also provide a useful insight into outbreaks around the world — and how different countries are faring in their efforts to bring coronavirus under control.
However, when comparing countries' growth factors, it's important to remember that the same number can mean different things depending on the severity of the outbreak and what stage it's at.
A growth factor of 0.99 in a country with thousands, or even tens of thousands of new cases each day represents a huge problem and a health system in ongoing crisis.
On the other hand, a growth factor of 0.99 in a country where new daily cases is quite low represents a much more manageable situation.
As an example, Australia's growth rate has been higher than the US for a month, but because we're coming from a much lower base we're in a completely different situation.
The following charts focus on the countries with the largest overall coronavirus outbreaks around the world, as well as some of Australia's nearest neighbours.
As you compare those global figures, it’s even more important to factor testing regimes into your thinking. If one country is testing a lot and another is testing very little, it's going to have a major impact on how their growth factors stack up.
What you need to know about coronavirus:
About the data
- Australian case numbers are sourced from federal, state and territory health department media releases and press conferences and compiled by ABC News. For countries other than Australia, the number of cases comes from data compiled by Johns Hopkins University.
- Health authorities update their figures at different times of day, so the numbers shown do not reflect the same point in time in each jurisdiction.
- Growth factors have been calculated by taking a seven day growth factor and converting it to daily terms.
- Where there are no new cases in the past seven days or the seven days prior to that, no growth factor is calculated. This is represented by a grey dotted line on the charts.
- It's important to note that all data in this story represents confirmed cases, which includes presumptive positive cases actually identified by authorities. The actual number of cases in each country is likely to be higher, as an unknown proportion of people with the virus would not have been tested. Therefore, the numbers' accuracy will also vary depending on how much testing each country is doing.
Credits
- Reporter & Developer: Simon Elvery
- Designer: Ben Spraggon
- Additional Reporting: Matt Martino
- Editor: Matt Liddy
- Australian data compiled by the ABC News Digital Story Innovations team
Editor's note: The methodology used to smooth out daily fluctuations in new cases was changed on Wednesday April 29 to more accurately represent growth factor changes, and to prevent too much weight from being given to some days in the smoothing window. The length of the smoothing window was also increased to seven days from five in order to eliminate the possibility that fewer tests being conducted on weekends might have an effect on reported case numbers in the following days. The period of time shown in the graphs was also increased.
Topics:covid-19, infectious-diseases-other, australia
First posted April 10, 2020 03:06:00
COVID research updates: Good timing might help the immune system to control COVID-19
22 September — Good timing might help the immune system to control COVID-19
People aged 65 and older who are infected with the new coronavirus tend to mount a disorganized immune response — a response that is also associated with severe COVID-19. This could help to explain why the disease strikes older people particularly hard.
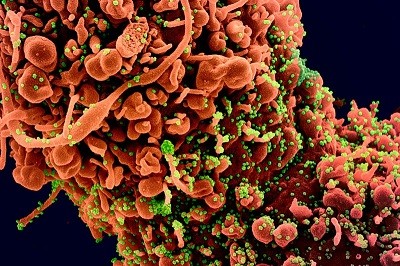
The immune system’s ‘adaptive’ branch, which targets specific invaders, has three principle components: antibodies, CD4+ T cells and CD8+ T cells. Alessandro Sette and Shane Crotty at the La Jolla Institute for Immunology in California studied the adaptive immune response in 24 people whose COVID-19 symptoms ranged from mild to fatal (C. R. Moderbacher et al. Cellhttps://doi.org/ghbwh7; 2020).

The team found that people whose immune systems failed to rapidly launch the entire adaptive immune system tended to have more severe disease than did people in whom all three arms ramped up production simultaneously. An uncoordinated response was particularly common among older people, and could indicate that both antibodies and T cells are important weapons against the coronavirus.
21 September — Business-class passenger spreads coronavirus on flight
Genetic evidence strongly suggests that at least one member of a married couple flying from the United States to Hong Kong infected two flight attendants during the trip.
Researchers led by Leo Poon at the University of Hong Kong and Deborah Watson-Jones at the London School of Hygiene & Tropical Medicine studied four people on the early-March flight (E. M. Choi et al. Emerg. Infect. Dis. https://doi.org/d9jn; 2020). Two were a husband and wife travelling in business class. The others were crew members: one in business class and one whose cabin assignment is unknown. The passengers had travelled in Canada and the United States before the flight and tested positive for the new coronavirus soon after arriving in Hong Kong. The flight attendants tested positive shortly thereafter.
The team found that the viral genomes of all four were identical and that their virus was a close genetic relative of some North American SARS-CoV-2 samples — but not of the SARS-CoV-2 prevalent in Hong Kong. This suggests that one or both of the passengers transmitted the virus to the crew members during the flight, the authors say. The authors add that no previous reports of in-flight spread have been supported by genetic evidence.
18 September — Musicians and a monk are tied to superspreading in Hong Kong
An estimated 19% of SARS-CoV-2 infections in Hong Kong seeded 80% of the local transmission of the virus from one person to another, according to an analysis of the virus’s early spread. The analysis also found that viral spread in social settings caused more infections than spread within family households.
In an examination of more than 1,000 coronavirus infections in Hong Kong from late January to late April, Peng Wu at the University of Hong Kong and her colleagues found evidence of multiple ‘superspreading’ events, in which one infected person passed the virus to at least six others (D. C. Adam et al. Nature Med. https://doi.org/d9c4; 2020). Musicians who performed at four Hong Kong bars are thought to have triggered the biggest cluster, which led to 106 cases. Another 19 cases were linked to a temple; one monk there had no symptoms but was found to be infected.
Nearly 70% of the cases did not transmit to anyone, the team found. The analysis also showed that more downstream cases were linked to spread in social settings such as weddings and restaurants than to household spread.
17 September — Immunity to common-cold coronaviruses is short-lived
Natural immunity to coronaviruses that cause the common cold might last for only a few months after infection, according to a study that monitored volunteers’ antibody levels — some for more than three decades.
Previous studies have suggested that immune responses to common-cold coronaviruses protect against reinfection for only a matter of months, although symptoms are often reduced during the second infection. Lia van der Hoek at the University of Amsterdam and her colleagues looked for coronavirus antibodies in blood samples taken every few months from ten individuals, starting in the mid-1980s (A. W. D. Edridge et al. Nature Med. https://doi.org/ghbm79; 2020).

The team used a rise in antibody levels as an indicator of infection. Infections with coronaviruses were least common from June to September, a seasonal pattern that the authors suggest SARS-CoV-2 might follow. The authors found reinfections occurring as early as 6 months after the first infection, and most often at 12 months.
15 September— A groundbreaking guide to making ‘cocktails’ to treat COVID-19
A new method pinpoints every mutation that a crucial SARS-CoV-2 protein could use to evade an attacking antibody. The results could inform the development of antibody treatments for COVID-19.
The immune system produces molecules called antibodies to fend off invaders. Antibodies that bind to an important region of the SARS-CoV-2 spike protein can inactivate the viral particles, making such antibodies attractive as therapies. But over time, viruses can accumulate mutations — and some can interfere with antibody binding and allow viral particles to ‘escape’ immune forces.
James Crowe at the Vanderbilt University Medical Center in Nashville, Tennessee, Jesse Bloom at the Fred Hutchinson Cancer Center in Seattle, Washington, and their colleagues created the most detailed map so far of the spike-protein mutations that could prevent binding by ten human antibodies (A. J. Greaney et al. Preprint at bioRxiv https://doi.org/d8zm; 2020). The team then used that information to design three antibody cocktails, each consisting of two antibodies.
In laboratory tests of the cocktails against SARS-CoV-2, the virus did not develop mutations that could escape antibody binding. The findings have not yet been peer reviewed.
14 September — Kids in US childcare centres spread coronavirus to families
Twelve children infected with the new coronavirus at childcare centres passed the virus on to at least another twelve people between them, according to an analysis of outbreaks in Utah. Among the resulting cases was a woman who had to be hospitalized after presumptive infection by her child.
Cuc Tran at the US Centers for Disease Control and Prevention in Atlanta, Georgia, and her colleagues investigated outbreaks at three childcare centres in Salt Lake County (Morb. Mortal. Wkly Rept. https://www.cdc.gov/mmwr/volumes/69/wr/mm6937e3.htm?s_cid=mm6937e3_w; 2020). At all three centres, the first known case was a staff member. Two had gone to work even though a person in their household had shown COVID-19 symptoms.
All 12 infected children, whose ages ranged from 8 months to 10 years, had either mild or no symptoms. Among the children’s close contacts who tested positive were six mothers and three siblings; one eight-month-old baby infected both parents. Not all close contacts were tested, meaning that infections associated with the childcare centres might have been missed, the authors say.
11 September —Nearly half of coronavirus transmission is from people not yet feeling ill
Some three-quarters of incidents of SARS-CoV-2 transmission occur in the few days before or after the onset of symptoms in the person who passes on the virus.
Luca Ferretti at the University of Oxford, UK, and colleagues studied 191 cases of SARS-CoV-2 transmission from an infected person to an uninfected person. The team analysed the timing of the transmitting person’s initial infection and onset of symptoms, and when that person spread the infection to someone else (L. Ferretti et al. Preprint at medRxiv https://doi.org/d8ms; 2020).
They found that roughly 40% of transmission events occurred before the onset of symptoms, and around 35% took place on the day that symptoms appeared or on the following day.
The researchers say their findings underscore the importance of mass testing, contact tracing and physical distancing to prevent transmission from pre-symptomatic people, as well as self-isolation for at least two days at the first sign of symptoms such as cough, fever, fatigue and loss of smell — however mild.
10 September — Surprise! A host of tantalizing new SARS-CoV-2 proteins is unveiled
Researchers have discovered nearly two dozen previously unknown proteins encoded by SARS-CoV-2 — and their role during infection is mostly mysterious.
Until now, SARS-CoV-2’s RNA genome was known to hold the instructions for making 29 proteins, such as the spike protein that helps viral particles to infect cells, and a variety of viral proteins that become active inside cells. But scientists were uncertain whether the virus had more than those 29.
To identify further proteins, Noam Stern-Ginossar at the Weizmann Institute of Science in Rehovot, Israel, and her colleagues sequenced SARS-CoV-2 RNA bound to protein-making machines called ribosomes inside infected cells (Y. Finkel et al. Naturehttps://doi.org/d8pb; 2020). This scan turned up 23 previously unknown proteins, including some that are entirely new and others that are shortened or extended versions of known proteins.
Some of the newfound proteins might control production of known viral molecules, but the role of many is unknown.
9 September — The immune-cell traits that could predict severe COVID-19
Immune cells called neutrophils are more likely to be primed for action in people who will eventually develop severe COVID-19 than in those who are will go on to become only mildly ill, according to a machine-learning analysis of data from 3,300 people. If the results can be reproduced, they could aid early identification of the people most likely to become critically ill.
Neutrophils comprise an important part of the body’s rapid response to infection, but can also damage uninfected tissue. Hyung Chun of Yale University in New Haven, Connecticut, and his colleagues used machine learning to analyse proteins in blood plasma taken from people hospitalized with COVID-19 (M. L. Meizlish et al. Preprint at medRxiv https://doi.org/d8hm; 2020).
Several immune proteins that are associated with neutrophils were found at higher levels in the plasma of people who later became critically ill than in those whose illness did not become severe. A subsequent analysis of health records from about 3,300 people showed that high neutrophil counts were associated with increased COVID-19 mortality. The findings have not yet been peer reviewed.
8 September — Kids ravaged by COVID-19 show unique immune profile
Most children infected with the new coronavirus show few signs of illness, if any. But a few children are struck by a severe form of COVID-19 that can cause multiple organ failure and even death. Now, scientists have begun to tease out the biology of this rare and devastating condition, called multisystem inflammatory syndrome in children, or MIS-C.
Doctors have diagnosed hundreds of cases of MIS-C, which shares some similarities with the childhood illness Kawasaki’s disease. To understand MIS-C’s biological profile, Petter Brodin at the Karolinska Institute in Stockholm and his colleagues looked at 13 children with MIS-C, 28 children with Kawasaki’s disease and 41with mild COVID-19 (C. R. Consiglio et al. Cellhttps://doi.org/d8fh; 2020). The researchers found that compared with children with Kawasaki’s disease, those with MIS-C have lower levels of an immune chemical called IL-17A, which has been implicated in inflammation and autoimmune disorders.
Unlike all the other children studied, children with MIS-C had no antibodies to two coronaviruses that cause the common cold. This deficit might be implicated in the origins of their condition, the authors say.
4 September — Powerful new evidence links steroid treatment to lower deaths
People severely ill with COVID-19 are less likely to die if they are given drugs called corticosteroids than people who are not, according to an analysis of hospital patients on five continents.
Earlier findings showed that the steroid dexamethasone cut deaths in people with COVID-19 on ventilators. To examine the effects of steroids in general, Jonathan Sterne at the University of Bristol, UK, and his colleagues did a meta-analysis that pooled data from seven clinical trials; each of the seven studied the use of steroids in people who were critically ill with COVID-19 (REACT Working Group J. Am. Med. Assoc.https://doi.org/d7z8; 2020). The trials included more than 1,700 people across 12 countries.
The team analysed participants’ status 28 days after they were randomly assigned to take either a steroid or a placebo. The risk of death was 32% for those who took a steroid and 40% for those who took a placebo. The authors say that steroids should be part of the standard treatment for people with severe COVID-19.
3 September — In a first, genomics shows that mink can pass SARS-CoV-2 to humans
An investigation of Dutch mink farms has found the first documented cases of animal-to-human transmission of SARS-CoV-2.
After SARS-CoV-2 outbreaks among farmed mink were first detected in late April, Marion Koopmans at Erasmus Medical Centre in Rotterdam, the Netherlands, and her colleagues used genome sequencing to track outbreaks among animals and workers at 16 mink farms (B. B. O. Munnink et al. Preprint at bioRxiv https://doi.org/d7xn; 2020). The team tested 97 farmworkers and their contacts, and found evidence for SARS-CoV-2 infection in 66 of them.
Genetic analysis suggested that workers had introduced SARS-CoV-2 to mink, which spread the virus back to workers, who might then have passed it on to other people. Outbreaks at mink farms have been detected in Denmark, Spain and the United States, and the researchers say unchecked spread could lead to the animals becoming a reservoir for human infections. The findings have not yet been peer reviewed.
2 September — Antibodies persist for months rather than dwindling
A sweeping survey in Iceland shows that antibodies against the new coronavirus endure in the body for four months after infection, countering earlier evidence suggesting that these important immune molecules quickly disappear.
After a pathogen invades, the immune system produces proteins called antibodies to fight off the intruder. Scientists do not know whether people who generate antibodies against SARS-CoV-2 are protected from reinfection, nor do they know how long those antibodies persist.
Kari Stefansson at deCODE Genetics–Amgen in Reykjavik and his colleagues measured the levels of SARS-CoV-2 antibodies in the blood of roughly 30,000 people, including more than 1,200 who had tested positive for the virus and recovered from COVID-19 (D. F. Gudbjartsson et al. N. Engl. J. Med.https://doi.org/gg9hbt; 2020). Roughly 90% of the recovered people had antibodies against the virus. Their antibody levels rose during the two months after diagnosis, plateaued and then remained at the same level for the duration of the study.
The results also show that the virus has infected only 0.9% of the population, leaving Iceland “vulnerable to a second wave of infection”, the authors warn.
1 September — Even octogenarians develop potent antibodies
As the new coronavirus ripped through several care homes in England, more than 80% of the residents mounted an antibody response to the virus, including 82% of those over the age of 80.

During outbreaks at six residential and nursing homes, Shamez Ladhani at Public Health England in London and his colleagues tested more than 500 residents and staff for SARS-CoV-2 infection (S. N. Ladhani et al. Preprint at medRxiv https://doi.org/d7p2; 2020). About five weeks later, the team tested many of the same people for antibodies to SARS-CoV-2 and in particular for neutralizing antibodies, potent molecules that can block the virus from infecting cells
The team found that roughly the same proportion of staff members and care-home residents had formed antibodies to the coronavirus. And neutralizing antibodies had developed in almost 90% of both staff members and residents, including more than 80% of people over the age of 80.
The authors caution that it is not clear whether antibodies against the virus guard against reinfection. The findings have not yet been peer-reviewed.
28 August ― COVID-19 testing helps sleep-away summer camps to avoid outbreaks
Rigorous SARS-CoV-2 testing and infection-control measures prevented outbreaks at four overnight camps in Maine that hosted hundreds of children between mid-June and mid-August.
Laura Blaisdell at the Maine Medical Center in Portland and colleagues report that the four sleep-away camps asked all attendees — both campers and staff — to be tested for SARS-CoV-2 before arrival (L. L. Blaisdell et al. Morb. Mortal. Wkly Rep. https://www.cdc.gov/mmwr/volumes/69/wr/mm6935e1.htm?s_cid=mm6935e1_w; 2020). Shortly after arrival, attendees were re-tested for the virus. They were also assigned to small cohorts and spent the first 14 days of camp quarantining with members of their cohort.
Of more than 1,000 attendees, 2 staff members and one camper tested positive at camp and were isolated until they tested negative. The 30 people in the camper’s cohort were quarantined; all tested negative for the virus during quarantine. The authors say that the virus did not spread beyond the three infected attendees.
27 August — Why infected primary-school pupils could be hard to spot
Children aged 6 to 13 are less likely to have symptoms of COVID-19 than those who are younger or older, according to a study of nearly 400 infected people under the age of 21.
Matthew Kelly and his colleagues at Duke University School of Medicine in Durham, North Carolina, studied 382 children and young adults who had had close contact with a person infected with SARS-CoV-2 (J. H. Hurst et al. Preprint at medRxiv http://doi.org/d7cb; 2020). Roughly three-quarters of the study participants tested positive for SARS-CoV-2 either before or during the study.
Only 61% of infected children aged 6 to 13 showed symptoms, compared with 75% of infected study participants under age 6 and 76% of those over age 13. Children aged 6–13 who did feel ill tended to have milder symptoms than older and younger study participants.
Nearly one-third of infected children with an infected sibling did not have close contact with an infected adult, implying that the virus had spread from child to child.
Screening systems at schools and day-care centres should account for age-related differences in symptoms, the authors say. The results have not yet been peer reviewed.
26 August — Sex differences in the COVID-19 immune response might drive men’s high risk
Variations in the immune response to SARS-CoV-2 could explain why men are more likely to be hospitalized and die of COVID-19 than are women.
Akiko Iwasaki at Yale University School of Medicine in New Haven, Connecticut, and colleagues studied the immune responses of 98 men and women infected with SARS-CoV-2. All had mild to moderate symptoms (T. Takahashi et al.Nature http://doi.org/d7gb; 2020). The researchers noticed that male participants’ typical immune response to infection differed from that of female participants, which could explain the more severe disease often observed in men. (Nature recognizes that sex and gender are neither binary nor fixed.)
The team found that in general, men had higher levels of certain inflammation-causing proteins known as cytokines and chemokines circulating in their blood than had women. By contrast, women tended to have a stronger response from immune cells known as T cells than did men. In men, an increase in symptom severity over time was associated with a weak T-cell response; in women, it was associated with increased amounts of inflammatory cytokines.
The study proposes taking sex into account when treating people with COVID-19.
25 August ― Reinfection with SARS-CoV-2 is confirmed for the first time with genetic evidence
A man in Hong Kong who was ill with COVID-19 in March was infected by a different variant of the new coronavirus several months later — the first evidence for reinfection that is supported by genetic analysis.

People infected with SARS-CoV-2 mount an immune response, which scientists think probably prevents most reinfections. The durability of this protection is unclear, and a documented case of reinfection would signal that immunity can wane. But previously reported reinfections have been found to relate instead to prolonged shedding of the virus or its genetic material
Kwok-Yung Yuen and his colleagues at the University of Hong Kong identified a 33-year-old man who recovered from COVID-19 in April and tested positive again more than 4 months later, after returning from Spain via the United Kingdom (K. K.-W. To et al. Clin. Infect. Dis.http://doi.org/d7ds; 2020). Genetic sequencing suggested that the second infection was caused by a virus that was genetically distinct from the one responsible for his initial bout.
The man never developed symptoms from the second infection, but his immune system responded by producing a fresh batch of antibodies.
21 August— Vaccines given through the nose could protect against infection
Studies in mice and monkeys show that nasal vaccinations can shield the animals from the new coronavirus — and that such vaccinations might be more effective than an injected form of the same vaccine.
David Curiel and Michael Diamond at Washington University School of Medicine in St Louis, Missouri, and their colleagues created a candidate vaccine encoding the SARS-CoV-2 spike protein, which the virus uses to invade cells (A. O. Hassan et al. Cellhttp://doi.org/d63k; 2020). The researchers then gave the vaccine to bioengineered mice that had human receptors for the protein.
After being injected with the vaccine and then exposed to SARS-CoV-2, mice showed no infectious virus in their lungs — but their lungs did harbour small amounts of viral RNA. By contrast, mice that had the vaccine inserted up their noses before exposure had no measurable viral RNA in their lungs. This and other evidence suggests that the nasal vaccine entirely warded off infection, the authors say.
Ling Chen at the First Affiliated Hospital of Guangzhou Medical University in China and colleagues developed another vaccine encoding the spike protein (L. Feng et al. Nature Commun. 11, 4207; 2020). The researchers found that both nasal and injected forms of the vaccine protected rhesus macaques (Macaca mulatta) from infection. The authors say that a vaccine that can be given by nose might allow people to vaccinate themselves.
20 August— A coronavirus mutation is tied to less severe illness
A SARS-CoV-2 mutation that appeared in East Asia early in the pandemic is linked to symptoms milder than those caused by the unmutated version of the virus.
In early 2020, researchers in Singapore identified a cluster of COVID-19 cases caused by a SARS-CoV-2 variant missing a chunk of RNA that spanned two genes, ORF7b and ORF8. To determine the consequences of this change, called a deletion, Lisa Ng at the Singapore Immunology Network and colleagues compared people infected with viruses carrying the deletion with those infected by normal viruses (B. E. Young et al. Lancethttp://doi.org/d6x7; 2020).
None of the 29 people whose viruses had the mutation needed supplemental oxygen, but 26 of the 92 people whose viruses lacked the mutation did. Viruses carrying the deletion haven’t been detected since March — possibly owing to infection-control measures.
The virus responsible for the 2002–04 outbreak of severe acute respiratory syndrome (SARS) acquired a similar deletion in the ORF8 gene, suggesting that this might be an important adaption to infecting humans, the authors say.
Correction: An earlier version of this article said researchers identified a SARS-CoV-2 variant missing a chunk of DNA.
19 August — An unprecedented map charts a key viral protein
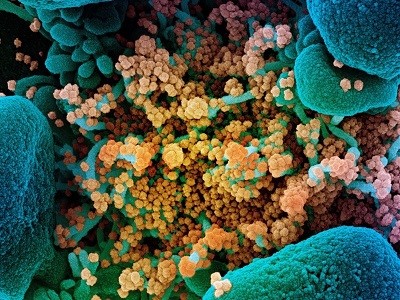
For the first time, researchers have mapped the 3D shape of spike proteins that are part of intact SARS-CoV-2 particles.
Spike proteins decorate the surface of coronaviruses and lock onto host receptors, such as ACE2, to gain entry to cells. The first structures of SARS-CoV-2’s spike were gleaned from modified proteins that had been expressed in cells and then purified. To check these models John Briggs at the Medical Research Council Laboratory of Molecular Biology in Cambridge, UK, and colleagues collected viral particles from infected cells and determined the shape of their spike proteins using electron microscopy (Z. Ke et al. Naturehttp://doi.org/d6sf; 2020).

These structures closely resembled the ones determined from purified forms. In both, the spike protein can adopt either a ‘closed’ confirmation or an ‘open’ one, which allows it to bind to a receptor. Studying the structure in viral particles could help to explain how spike-binding antibodies block infection, the researchers say.
17 August — Sailors furnish first evidence that antibodies protect humans against re-infection
A massive COVID-19 outbreak on a US fishing boat spared crew members who already had antibodies against the new coronavirus, providing what scientists say is the first direct evidence that these antibodies protect people against being reinfected.
After a viral infection, the immune system makes compounds called neutralizing antibodies that can attack the virus if it invades again. But previous research had not determined whether such antibodies can shield humans from SARS-CoV-2 reinfection.

Alexander Greninger at the University of Washington School of Medicine in Seattle and his colleagues tested the crew of a US fishing vessel for SARS-CoV-2 and for antibodies to the virus (A. Addetia et al. Preprint at medRxiv http://doi.org/d6qm; 2020). Just before the ship’s departure, the researchers tested 120 of the 122 crew members and found that all were negative for SARS-CoV2, but an outbreak hit the ship soon after it left shore.
Post-voyage testing showed that 104 members of the 122-person crew were infected. None of those who were infected and had been tested before embarking had shown neutralizing antibodies against SARS-CoV-2.
But all three crew members who did have such antibodies before departure escaped infection, providing statistically significant evidence that neutralizing antibodies acquired during SARS-CoV-2 infection protect against reinfection, the authors say. The findings have not yet been peer reviewed.
7 August — For fast and low-cost COVID-19 testing, just spit
A quick, cheap and painless test that detects SARS-CoV-2 RNA in spit could be used for mass testing.
Chantal Vogels at Yale School of Medicine in New Haven, Connecticut, and colleagues developed a simple saliva test — called SalivaDirect — to address the growing demand for extensive testing as lockdowns lift (C. B. F. Vogels et al. Preprint at medRxiv http://doi.org/d5s3; 2020).
Compared with the gold-standard nose and throat swab, the saliva test is less invasive, does not need to be conducted by a trained professional and avoids the use of scarce chemicals that are needed to store and extract viral RNA. In validation experiments, SalivaDirect detected 32 out of 34 samples that tested positive in nose and throat swabs, and 30 out of 33 negative samples.
The researchers estimate a cost-per-spit of US$1.29–$4.37, and have requested that the United States Food and Drug Administration authorize the test for emergency use.
6 August — Immune reaction to some common colds might provide protection
Some immune cells that recognize coronaviruses that cause the common cold also respond to SARS-CoV-2, the coronavirus responsible for the COVID-19 pandemic.
Previous studies have found that some people who have never been exposed to SARS-CoV-2 nevertheless have immune cells called memory T cells that can recognize the virus. Daniela Weiskopf and Alessandro Sette at the La Jolla Institute for Immunology in California analysed such T cells, and found that they recognize particular sequences of several SARS-CoV-2 proteins (J. Mateus et al. Sciencehttp://doi.org/d5v5; 2020).
The team then identified similar sequences in common-cold coronaviruses, and showed these sequences could activate some T cells that also respond to SARS-CoV-2. The findings add weight to the hypothesis that existing immunity to cold coronaviruses could contribute to differences in COVID-19 severity, but further studies are required to support that conclusion.
5 August — Antibody blend protects monkeys and hamsters from viral symptoms
A mixture of two human antibodies against the new coronavirus shows promise in animal tests for preventing and treating COVID-19.
Neutralizing antibodies are immune molecules that can attach to viruses and disable them. Christos Kyratsous at Regeneron Pharmaceuticals in Tarrytown, New York, and his colleagues made a cocktail of two neutralizing antibodies that bind SARS-CoV-2. They gave the cocktail to rhesus macaques (Macaca mulatta), which become mildly ill when infected.

The researchers found that compared to animals that took a placebo, monkeys that received the antibody combination were less likely to develop pneumonia and, if they did, had less lung damage. This was true in monkeys that took the antibodies either before or after receiving a dose of the virus (A. Baum et al. Preprint at bioRxiv http://doi.org/d5r9; 2020).
Unlike macaques, Syrian golden hamsters (Mesocricetus auratus) infected with SARS-CoV-2 become acutely ill. But hamsters dosed with virus lost less weight — or even gained weight — compared with control rodents if given the antibody cocktail before or after receiving a dose of the virus. The findings have not yet been peer reviewed.
3 August — Summer-camp outbreak infects more than 200 children
Despite measures to prevent the spread of the new coronavirus, at least 250 campers and staff members tested positive for SARS-CoV-2 after attending an overnight camp in the US state of Georgia.
Christine Szablewski at the Georgia Department of Public Health in Atlanta and her colleagues investigated the outbreak, which began two days after the first campers’ arrival on 21 June (C. M. Szablewski et al. Morb. Mortal. Wkly Rep. http://doi.org/d5ms; 2020). All campers and staff were required to test negative for the virus fewer than 13 days before arrival, and campers did not mix with those sleeping in other cabins. Campers were not required to wear masks.
The researchers found that nearly 100 staff members — many of them teenagers — tested positive in the two weeks after leaving camp. So did 168 campers, including half of those aged between 6 and 10. Factors contributing to the outbreak included the large number of campers sleeping in each cabin and what the researchers describe as “daily vigorous singing and cheering”.
30 July — Vaccine candidate protects monkeys from infection
An experimental coronavirus vaccine seems to have completely prevented infection in most monkeys that received the jab.
Hanneke Schuitemaker at Janssen Vaccines and Prevention in Leiden, the Netherlands, Dan Barouch at Beth Israel Deaconess Medical Center in Boston, Massachusetts, and their colleagues gave 32 rhesus macaques (Macaca mulatta) a single dose of one of 7 vaccines (N. B. Mercado et al. Naturehttp://doi.org/d5d4; 2020). Each vaccine comprised a weakened respiratory virus coding for one of seven forms of SARS-CoV-2’s spike protein.
After vaccination, nearly all the monkeys made neutralizing antibodies — powerful immune molecules that can block infection — and T cells that trigger other immune responses. When monkeys were exposed to SARS-CoV-2, the most potent of the vaccines prevented lung infection in six out of six animals that received it, and nasal infection in five out of six.
Across all the vaccinated monkeys, levels of neutralizing antibodies were associated with protection from SARS-CoV-2 infection, but levels of T cells were not.
29 July— Immune cells against the virus are found in unexposed people
Immune cells called T cells are prepared to attack the new coronavirus not only in people with COVID-19, but also in some who have not been exposed to the virus.
At first, researchers studying the immune response to SARS-CoV-2 focused mostly on the immune molecules called antibodies, but T cells offer another possible route to immunity. Andreas Thiel at Charité University Hospital Berlin and his colleagues surveyed blood samples for T cells that react to the SARS-CoV-2 spike protein (J. Braun et al. Naturehttp://doi.org/d5bv; 2020).

The team found such cells in 83% of study participants with COVID-19, as well as 35% of healthy blood donors who had not been exposed to SARS-CoV-2. The authors speculate that the reactive T cells might have been generated in healthy donors during past infections with related coronaviruses, but it remains unclear whether these cells offer protection against SARS-CoV-2.
28 July — Mutations allow virus to elude antibodies
Mutations in SARS-CoV-2 might help the virus to thwart potent immune molecules.
The blood of many people who recover from COVID-19 contains immune-system molecules called neutralizing antibodies that disable particles of the new coronavirus. Most such antibodies recognize the new coronavirus’s spike protein, which the virus uses to infect cells. Researchers hope that these molecules can be used as therapies, and can be elicited by vaccines.
Theodora Hatziioannou and Paul Bieniasz at the Rockefeller University in New York City and their colleagues engineered a version of the vesicular stomatitis virus, which infects livestock, to make the spike protein. They then grew the virus in the presence of neutralizing antibodies (Y. Weisblum et al. Preprint at bioRxiv http://doi.org/d439; 2020). The spike protein in the engineered viruses acquired mutations that allowed the viruses to escape recognition by a range of neutralizing antibodies.
The team also found these mutations in SARS-CoV-2 samples from infected people around the world, although at very low frequencies. Treatment ‘cocktails’ of multiple neutralizing antibodies, each recognizing a different part of the spike protein, could stop the virus from evolving resistance to these molecules, the authors suggest. The findings have not yet been peer reviewed.
27 July— The power of China’s virus-control campaign is seen in pattern of symptoms
In China, a key metric of epidemics called the serial interval shrank drastically soon after the new coronavirus’s arrival — a finding that underscores the success of China’s testing and isolation efforts.
The serial interval is the average time between the onset of symptoms in a chain of people infected by a pathogen. Benjamin Cowling at the University of Hong Kong and his colleagues modelled the spread of SARS-CoV-2 in China and found that the serial interval plummeted from 7.8 days to 2.6 days over a 5-week period starting on 9 January (S. T. Ali et al. Sciencehttp://doi.org/gg5mpc; 2020).
The researchers say that early isolation of cases prevented transmission that would otherwise have occurred later in an infectious period, leading to fewer cases and slowing the spread of the virus. As a result, most of the remaining transmissions occurred either before infected people showed symptoms or early in the symptomatic phase, and the serial interval shrank.
The authors suggest the serial interval distribution be used in real time to track the changing transmissibility of the virus.
24 July — Dogs’ and cats’ infection rates mirror those of people
Cats and dogs are just as likely to be infected with SARS-CoV-2 as people are, according to a survey in northern Italy that is the largest study of pets so far.
Nicola Decaro at the University of Bari and his colleagues took nose, throat or rectal swabs of 540 dogs and 277 cats in northern Italy between March and May (E. I. Patterson et al. Preprint at bioRxiv http://doi.org/d4r7; 2020). The animals lived in homes with infected people, or in regions severely affected by COVID-19.
None of the pets tested positive for SARS-CoV-2 viral RNA, but in further tests of antibodies against the virus circulating in the blood of some animals, the researchers found that around 3% of dogs and 4% of cats showed evidence of previous infection.
Infection rates among cats and dogs were comparable with those among people in Europe at the time of testing, suggesting that it is not unusual for pets to be infected. The findings have not yet been peer reviewed.
24 July — Virus rips through Israeli school after masking is suspended
More than 150 students at an Israeli secondary school were infected by the new coronavirus after students were allowed to remove their masks during a heat-wave.
Roughly 10 days after Israeli schools fully reopened on 17 May, two students at a secondary school in Jerusalem were diagnosed with COVID-19. Chen Stein-Zamir at the Ministry of Health in Jerusalem and her colleagues investigated the resulting outbreak and found that 153 students and 25 members of staff had become infected (C. Stein-Zamir et al. Euro Surveill.http://doi.org/d4sw; 2020). By mid-June, a further 87 cases had occurred among the close contacts of people infected through the school outbreak.

The virus’s spread was probably aided by a heat-wave that occurred between 19 and 21 May, prompting heavy use of air-conditioning and a suspension of the requirement that students wear face masks. Crowding might also have contributed: each of the school’s classrooms held 35 to 38 students, resulting in space allotments of 1.1–1.3 square metres per student.
22 July — Severely ill people yield diverse trove of powerful antibodies
Scientists have identified a diverse group of antibodies that block the new coronavirus’s ability to infect cells — even when applied in low doses.
The immune-system proteins called neutralizing antibodies interfere with hostile microbes trying to enter target cells. David Ho at Columbia University Vagelos College of Physicians and Surgeons in New York City and his colleagues studied neutralizing antibodies from the plasma of five people with severe cases of COVID-19 (L. Liu et al. Naturehttp://doi.org/d4md; 2020).
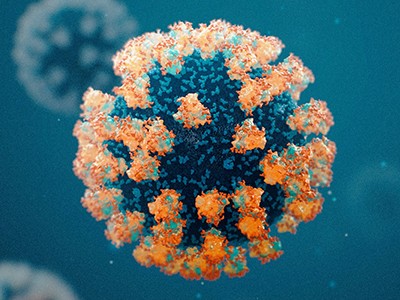
Nineteen antibodies proved highly effective at preventing SARS-CoV-2 infection of cell samples. A small dose of one of the antibodies protected golden Syrian hamsters (Mesocricetus auratus) from SARS-CoV-2 infection.
The 19 antibodies attach to a variety of locations on the coronavirus spike protein. A therapy made from antibodies that fasten onto the spike protein at multiple sites could be difficult for the virus to evade through mutation.
21 July — Viral levels could help to target treatment
The amount of viral RNA in the nose and throat of a person infected with the new coronavirus could help clinicians to decide how best to treat them, according to an analysis of thousands of swabs taken at a hospital in Switzerland.
Onya Opota and his colleagues at Lausanne University Hospital analysed the viral load — the amount of virus in a standard volume of material — of samples taken from 4,172 people infected with SARS-CoV-2 between 1 February and 27 April (D. Jacot et al. Preprint at medRxiv http://doi.org/d4b8; 2020). They noticed two distinct stages of COVID-19. Early in the disease, people have high viral loads, which tend to decline gradually as the disease progresses. This later stage is typically characterized by inflammation. The decline of viral loads could thus serve as a cue to start treating infected people with anti-inflammatory drugs.
But the researchers found no correlation between viral load and the severity of disease, suggesting that it is not a good predictor of a patient’s outcome. The research has not yet been peer reviewed.
16 July — Antiviral antibodies peter out within weeks after infection
Key antibodies that neutralize the effects of the new coronavirus fall to low levels within months of SARS-CoV-2 infection, according to the most comprehensive study yet.
Neutralizing antibodies can block a pathogen from infecting cells. But such antibody responses against coronaviruses often wane after just a few weeks.

Katie Doores at King’s College London and her colleagues monitored the concentration of neutralizing antibodies against SARS-CoV-2 in 65 infected people for up to 94 days (J. Seow et al. Preprint at medRxiv http://doi.org/d3s2; 2020). In a preprint that has not yet been peer reviewed, the team reports that at the peak of antibody production, people with severe COVID-19 symptoms had higher levels of antibodies than had people with mild disease.
However, in most people, antibody levels began to fall about a month after symptoms appeared, sometimes to nearly undetectable levels — raising questions about the durability of vaccines designed to promote the production of neutralizing antibodies.
15 July — Positive trial results raise hopes for a top vaccine candidate
A leading COVID-19 vaccine candidate generates an immune response against the virus and causes few side effects, according to preliminary data from a phase I safety study with 45 participants.
The vaccine is being co-developed by Moderna in Cambridge, Massachusetts, and the US National Institute of Allergy and Infectious Diseases. It consists of RNA instructions that prompt human cells to make the virus’s spike protein, generating an immune response.

Lisa Jackson at Kaiser Permanente Washington Health Research Institute in Seattle and her colleagues gave participants two injections, administered four weeks apart, of one of three different doses of the vaccine (L. A. Jackson et al. N. Engl. J. Med. http://doi.org/d3tt; 2020). Most side effects were mild, although three participants who got the highest dose experienced worse complications, such as a high fever.
After the injections, all participants produced immune proteins called antibodies capable of recognizing the SARS-CoV-2 virus, as well as ‘neutralizing antibodies’ that can block infection. A 30,000-participant phase III trial to test whether the vaccine can prevent COVID-19 is set to begin in late July.
15 July — Severe COVID-19 has a telltale immune profile
Scientists have identified an immune-system signature in people with serious COVID-19 — a finding that could inform the development of treatments for the disease.

Benjamin Terrier at the University of Paris and his colleagues analysed blood samples from 50 people infected with SARS-CoV-2 (J. Hadjadj et al.Sciencehttp://doi.org/gg4vjx; 2020). Compared to the individuals with mild or moderate symptoms, those with severe disease produced fewer antiviral proteins called interferons and more inflammatory molecules. The researchers also found that blood levels of a specific interferon decreased just before participants had to be taken to intensive-care units.
The results suggest that reduction of interferon levels in the blood is a hallmark of severe COVID-19. Treatments that counter inflammation and increase levels of interferons could help people with the disease, the researchers say.
13 July — Virus’s US invasion might have started in 2019
The new coronavirus spread across much of the interior of the United States by tagging along with people moving from state to state, but US coastal regions were seeded with SARS-CoV-2 imported from other countries — perhaps in 2019, according to models.
Alessandro Vespignani at Northeastern University in Boston, Massachusetts, and his colleagues studied air traffic, commuting patterns and other data to understand how and when the coronavirus took hold in the United States (J. T. Davis et al. Preprint at medRxiv http://doi.org/d3mf; 2020). The team found that in several coastal states, international travel drove introduction of the virus. In California and New York, SARS-CoV-2 might have begun circulating as early as December 2019.

But in many non-coastal states, domestic travellers rather than international visitors were the source of the first wave of infections. Infections spread across the country from late January to early March but were largely undetected, the authors say. The findings have not yet been peer reviewed.
10 July — Massive contact-tracing effort finds hundreds of cases linked to nightclubs
Mobile phone and credit card data helped to identify nearly 250 coronavirus infections linked to a fast-moving outbreak that began in a popular nightclub district in Seoul.
Soon after South Korean nightclubs reopened 30 April, public-health officials noted a cluster of COVID-19 cases among people who had visited Seoul’s Itaewon club district. Jin Yong Lee at Seoul National University Boramae Medical Centre and his colleagues used mobile phone location data, credit card payment records and other information to identify more than 60,000 people who had spent time in or near Itaewon clubs (C. R. Kang et al. Emerg. Infect. Dis. http://doi.org/gg4fhj; 2020) in late April or early May. All were encouraged to undergo testing for SARS-CoV-2.
By late May, officials had tested more than 40,000 people. The effort turned up 246 infections — including several that were 3, 4 and even 5 steps along the transmission chain from club-goers.
What’s New in the Coronavirus serial key or number?
Screen Shot
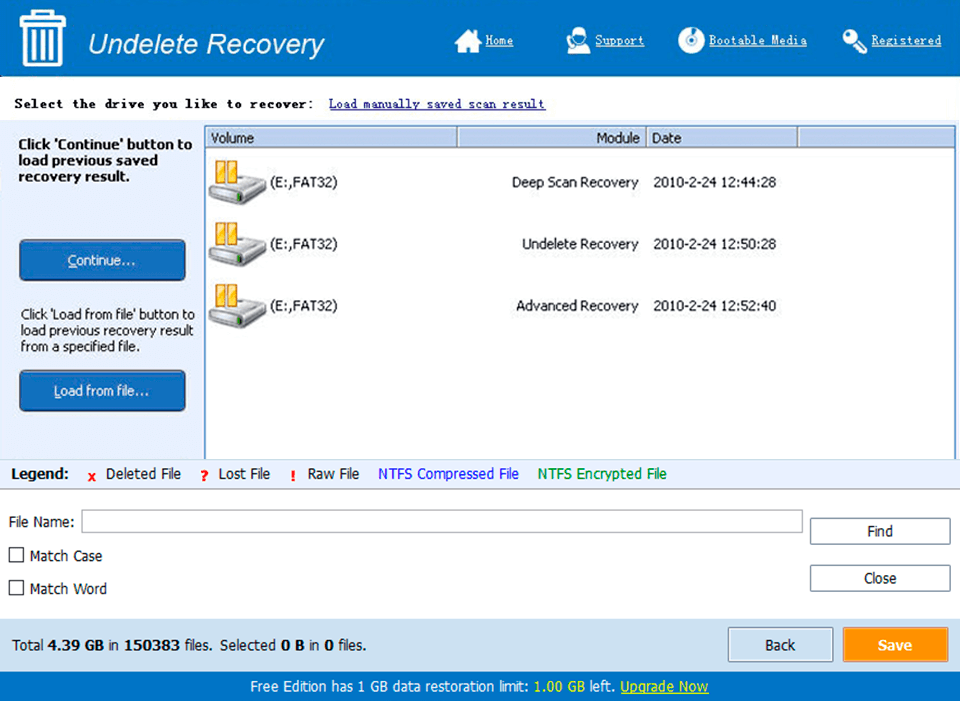
System Requirements for Coronavirus serial key or number
- First, download the Coronavirus serial key or number
-
You can download its setup from given links:


